For more information on the novel coronavirus and Covid-19, visit cdc.gov.
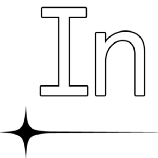
Approximately one in four people with diabetes are using less insulin than they need because of the cost
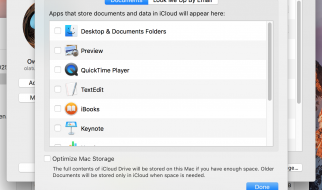
 Photo: Erik McGregor/LightRocket/Getty Images
Photo: Erik McGregor/LightRocket/Getty Images
 In the past 10 years, the price of insulin in the United States has tripled. For those people with diabetes who have to buy their insulin without insurance or with high-deductibles and coinsurance plans, the inflated price of this essential drug has forced impossible choices between buying insulin and paying for rent or buying food. (In some cases, biohackers with diabetes are even making their own insulin.)
In the past 10 years, the price of insulin in the United States has tripled. For those people with diabetes who have to buy their insulin without insurance or with high-deductibles and coinsurance plans, the inflated price of this essential drug has forced impossible choices between buying insulin and paying for rent or buying food. (In some cases, biohackers with diabetes are even making their own insulin.)
In one 2019 study, one in four people with diabetes reported using less insulin than they needed because of the cost. This can impact blood sugar levels and lead to long-term consequences like blindness and amputations. For people with Type 1 diabetes like me, going without insulin ultimately leads to death.
As I write this, I?m reading about people resorting to shady deals on Craigslist to be able to afford their insulin. The other week the headlines were about a bus Bernie Sanders chartered to take people to buy their insulin in Canada. And tragic stories continue to surface of people with diabetes who have died rationing insulin because they were unable to afford it.
As I write this, I?m reading about people resorting to shady deals on Craigslist to be able to afford their insulin.
The great irony of all this is that the scientists who discovered insulin never intended to profit from it. After winning the 1923 Nobel Prize, they sold the patent for insulin to the University of Toronto for $3. One of the scientists, Frederick Banting, famously said, ?Insulin does not belong to me, it belongs to the world.? In that first year, so many patients wanted the new medicine that insulin had to be rationed until they could sort out the manufacturing process. A century later people are rationing insulin once again. What happened?
The reasons for the increasing cost of insulin in the U.S. are complex, but according to a recent article in the New England Journal of Medicine, it comes down to two major factors: lack of pricing regulations and lack of competition.
Under U.S. law, pharmaceutical manufacturers can set any price they wish for their products. Insulin prices are set based on an arcane system of discounts and rebates which flow between entities in the insulin supply chain. It?s an extraordinarily opaque system. Even the American Diabetes Association Working Group on the issue struggled to explain the role of every link in the supply chain in the skyrocketing price of insulin.
The upshot is that the current system creates incentives to increase the ?list price? of insulin ? which is the price set by the manufacturer ? as much as possible. Insulin manufacturers have argued that the list price does not reflect what patients actually pay after all the rebates and discounts have kicked in, but people without insurance or who end up in other coverage gaps ? such as the Medicare ?donut hole? ? are exposed to the full list price.
For the insulin I use, Eli Lilly?s Humalog, the list price is $332 per vial, which is what I would pay if I wasn?t insured. I usually use two or three vials per month. Other people with diabetes might require substantially more. It adds up fast. When Humalog came out in 1996, one vial cost $21.
Further, because there are no generic insulins ? called ?biosimilars? ? to compete with the brand-name insulins, prices are allowed to swell without checks or balances.
That lack of competition isn?t an accident. Though the original patents for most of the insulin formulations on the market expired years ago, the big three insulin manufacturers have extended their monopolies by patenting incremental changes to their products and manufacturing processes. Those patents can then be used to tie-up potential generic competitors in long, costly legal battles. In addition, they have been shielded from competition from generics by stringent federal regulations around ?biologics? like insulin, which is a complex molecule produced by living cells. These make it more challenging for generic insulins to enter the market.
Some numbers:
- The average ?list price? of the most common insulins in the U.S. has increased by more than 700% (after inflation) in the past two decades. A 10-milliliter vial that cost $20 in the ?90s now costs more than $250 without insurance.
- Though there is wide variation in cost due to differences in insurance, types of insulin used, and amount of insulin used, in 2016, the average annual cost of insulin for a person with Type 1 diabetes in the U.S. was $5,705, more than double what it was in 2012. In general, people with diabetes spend on average 2.3 times more on health care than people without diabetes.
- Insulins in the U.S. on average cost more than 10 times as much as the same products in other developed countries.
- About 90% of the insulin sold in the U.S. is manufactured by the same three companies ? Eli Lilly, Novo Nordisk, and Sanofi.
Under pressure from #insulin4all advocates, patients, doctors, and politicians, some companies have taken steps to reduce the price of insulin ? such as Eli Lilly?s recent release of a half-price ?authorized generic? insulin and Cigna?s Express Scripts? $25 cap on insulin co-pays ? but these do not do enough to address the issue. The ?half-price? Humalog ($137.35 for a single vial) is still much more expensive than even the brand-name version in Germany ($55) or Canada ($32). The Cigna offer does nothing to help people who do not have insurance.
Government, too, is scrambling to address the problem. In my home state of Colorado, for example, a recent law to limit monthly co-payments for insulin to $100 was the first to be passed in the country, though the law only covers people with insurance and is likely to increase monthly premiums. A number of federal measures have also been proposed to address insulin affordability. They include the creation of insulin assistance programs, lowering barriers to entry for generic insulins, formalizing imports of insulin from other countries, and creating regulation to set insulin prices based on international reference prices. But despite apparent bipartisan agreement that drugs are too expensive, the federal legislative fixes have stalled.
In the meantime, people will continue to struggle to afford the insulin they require to live and to be healthy. Assuming there?s not room for everyone on Bernie?s bus to Canada, the best bet for affordable insulin right now might be Craigslist.
Banting is turning in his grave.