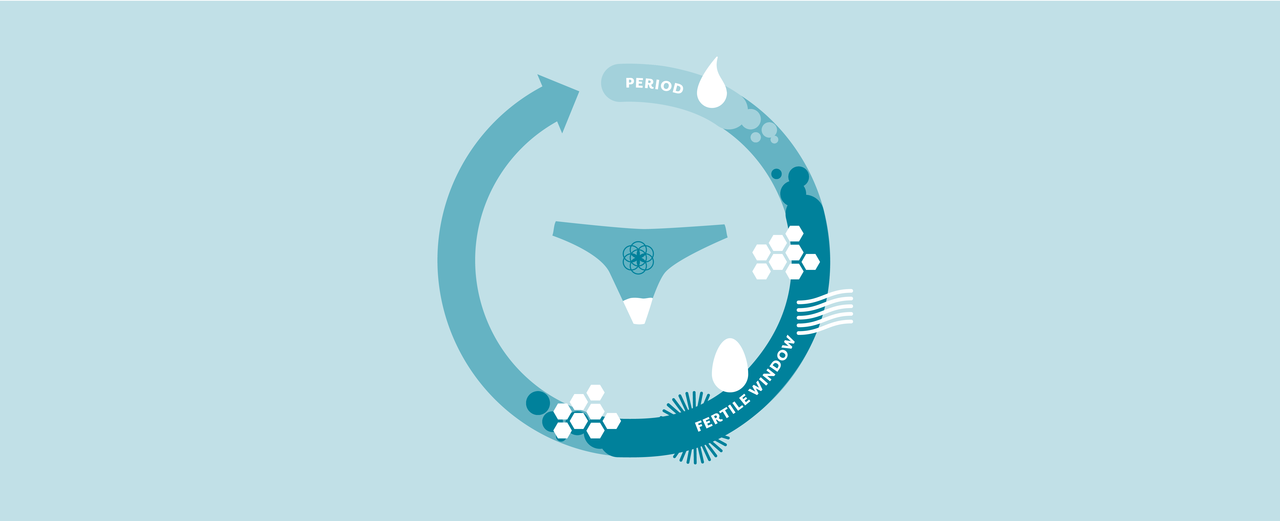
Tracking your cervical fluid can give you clues about what hormonal changes and events are happening in your body right now. Understanding your own patterns can help you to know when ovulation has occurred, and when you might be able to skip the lube. Getting to know your fluid can also allow you to recognize when something may be off ? from an infection or hormonal issue, for example.
The ebbs and flows of cervical fluid
The cervix is the passageway between your lower and upper reproductive tract. It has glands in and around it which produce fluid. The quality, consistency, and volume of this fluid changes along with your cycle. The pattern and experience of these changes is different for everyone but cervical fluid tends to follow a consistent cyclical pattern. It changes in quality, quantity and function. This happens in response to your changing hormones. At different times, cervical fluid acts to facilitate or prevent sperm from moving past your cervix (1). It also contains antibodies, and helps to keep out unhealthy bacteria and viruses (2).
A fluid timeline
1. Menstruation: Start of cycle
On day one of the cycle, both estrogen and progesterone are low. The cervix is not likely producing much fluid, but you won?t be able to tell, as it?s mixed in with blood, endometrial tissue and dissolved remnants of a disintegrated egg.
2. Dry/Sticky: Early-to-mid follicular phase
In the early follicular phase, estrogen starts to rise (it?s produced by your follicles as they grow). This leads to an increased production of fluid. You probably won?t notice much of it in the days after your period ? these are ?dry? fluid days for many people ? some might notice ?sticky? fluid. Typically, cervical fluid first becomes noticeable around the middle of the follicular phase (day ~7 in a 28 day cycle) (3).
3. Creamy: Mid-to-late follicular phase
It may start sticky, but as estrogen and water content rises fluid tends to become ?creamy,? cloudy (not clear) and whitish or yellowish. Research has shown sperm can start to swim through cervical fluid on about day ~9 of a 28 day cycle (1).
4. Egg White/Wet: Late follicular phase/mid-cycle
As ovulation approaches, more cervical fluid is produced. Fluid becomes stretchier, clearer and more wet and slippery ? like an raw egg white. This fluid tends to ?peak? about 1?2 days before ovulation, when estrogen is highest (3). Around that time fluid can often be stretched several inches between your finger and thumb. For others it may be more watery. The amount of peak fluid the body produces is different for everyone, but it can be up to 20x more in some cases (4). This fluid is about 95% water by weight, and 5% solids (electrolytes, organic compounds and soluble proteins)(2). If you?re having sex and using lube, you may notice you need less around this time. *Note that the presence of fertile-type cervical fluid alone cannot confirm ovulation ? it?s not accurate enough on its own to use for a FAM method or pregnancy prevention.
5. Dry/Sticky: Luteal phase
As soon as ovulation is over, your fluid changes. Even before you notice a visual change, it will already have become more fibrous and less penetrable for sperm (1). In the day or two after ovulation (the first days of the luteal phase), cervical fluid lessens and becomes much thicker. Progesterone, the dominant hormone in this phase, acts to inhibit the secretion of fluid from the epithelial cells (1). You may notice little fluid, or it may be sticky (or something else unique to you).
Note that every body is unique ? these changes may show up differently for you, or you may experience or interpret them in a different way.
To swim or stick ? the changing role of fluid
So why does cervical fluid change so much? Each change serves its own function. Cervical fluid during the fertile window is built to provide sperm with a buffer from the slight acidity of the vagina. The change in fluid consistency also allows for heightened antimicrobial action (5). Sperm that enters the vagina before ovulation can be suspended in this fluid, increasing its survival and likely heightening the chance that it will be around when ovulation happens (1). ?Fertile? fluid is most facilitating of sperm travel ? but not too facilitating. This fluid also acts as one way to filter in the ?best? sperm (6, 7). Slower swimmers get left behind, as does sperm with other motility or structural differences (5). Only a minority of sperm actually make it to the uterus (8).
When ovulation is over, and the window of potential pregnancy has closed, cervical fluid becomes a barrier to sperm entering the upper reproductive tract. The progesterone in your luteal phase acts just like the progesterone in a mini-pill (progesterone-only birth control pills). Its viscosity (aka thick, sticky texture) makes it so sperm cannot get past the cervix. This helps to prevent bad bacteria/viruses from entering as well.
This leads us back to menstruation, and the cycle begins again?
References
- World Health Organisation. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge university press; 1999 May 13.
- Saltzman WM, Radomsky ML, Whaley KJ, Cone RA. Antibody diffusion in human cervical mucus. Biophysical journal. 1994 Feb 1;66(2):508?15.
- Bigelow JL, Dunson DB, Stanford JB, Ecochard R, Gnoth C, Colombo B. Mucus observations in the fertile window: a better predictor of conception than timing of intercourse. Human Reproduction. 2004 Apr 1;19(4):889?92.
- Moriyama A, Shimoya K, Ogata I, Kimura T, Nakamura T, Wada H, Ohashi K, Azuma C, Saji F, Murata Y. Secretory leukocyte protease inhibitor (SLPI) concentrations in cervical mucus of women with normal menstrual cycle. Molecular human reproduction. 1999 Jul 1;5(7):656?61.
- Sakkas D, Ramalingam M, Garrido N, Barratt CL. Sperm selection in natural conception: what can we learn from Mother Nature to improve assisted reproduction outcomes?. Human reproduction update. 2015 Nov 1;21(6):711?26.
- Katz DF, Drobnis EZ, Overstreet JW. Factors regulating mammalian sperm migration through the female reproductive tract and oocyte vestments. Gamete research. 1989 Apr 1;22(4):443?69.
- Yudin AI, Hanson FW, Katz DF. Human cervical mucus and its interaction with sperm: a fine-structural view. Biology of reproduction. 1989 Mar 1;40(3):661?71.
- Suarez SS, Pacey AA. Sperm transport in the female reproductive tract. Human reproduction update. 2006 Jan 1;12(1):23?37.