The Science behind 50% of our population.
We?ve been milking cows for the last 8,000 (ish) years.
Why the first cow-milker decided to fiddle with a 2000 pound animal?s breast is a great question. But hey, we have milk, cheese and factory farming because of it!
In contrast, we?ve been ?milking humans? for about 200,000 years (25X longer).
Orwell H. Needham patented the first ?real? breast pump for women in 1854. He designed it with inspiration from a cow-milking machine.
We created a device to milk cows before we created a device to milk women. And women didn?t design it; Orwell was a man.
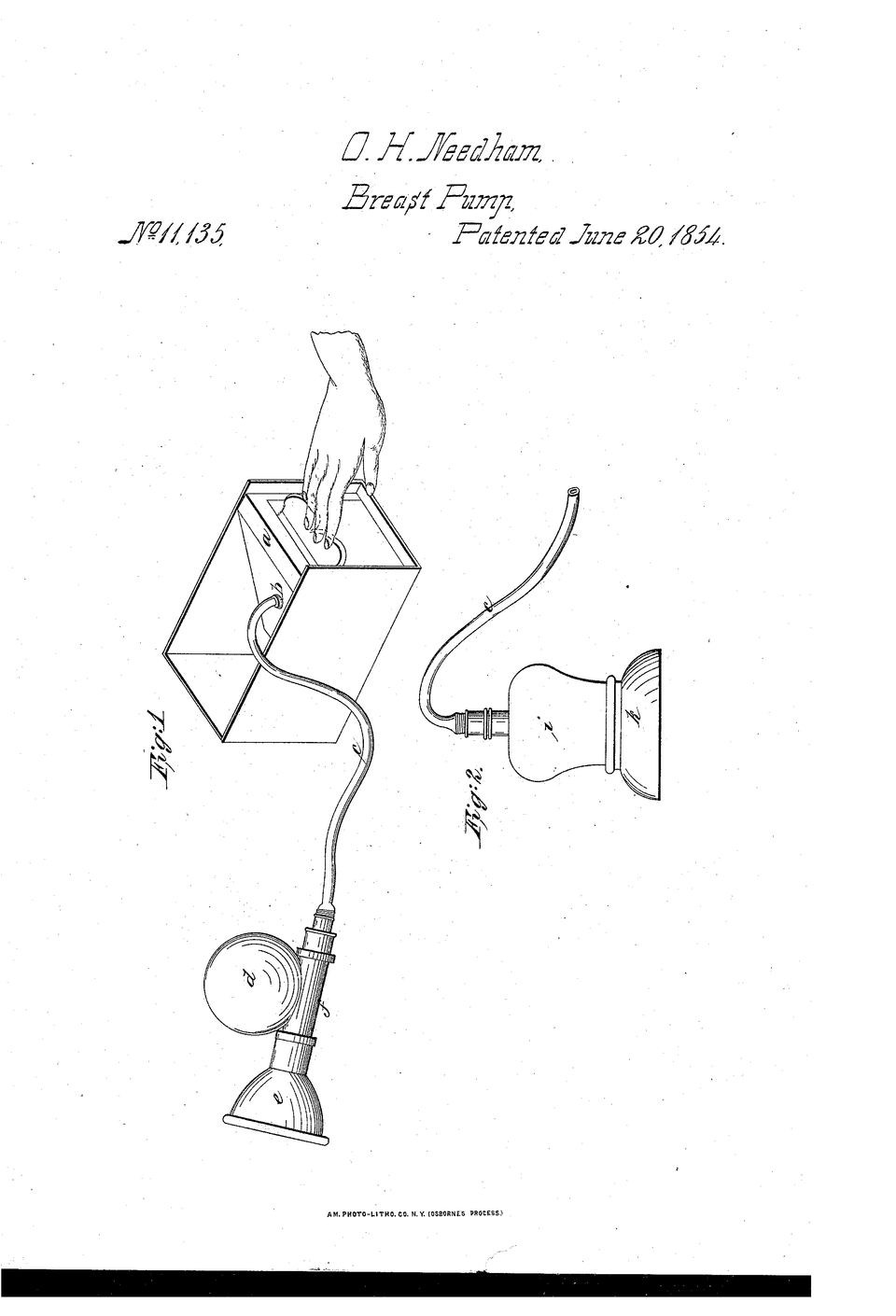 `The first breast pump. No, it?s not supposed to be user friendly, intuitive or comfortable.
`The first breast pump. No, it?s not supposed to be user friendly, intuitive or comfortable.
The next iteration of the breast pump was in 1874, 20 years later, by 2 men.
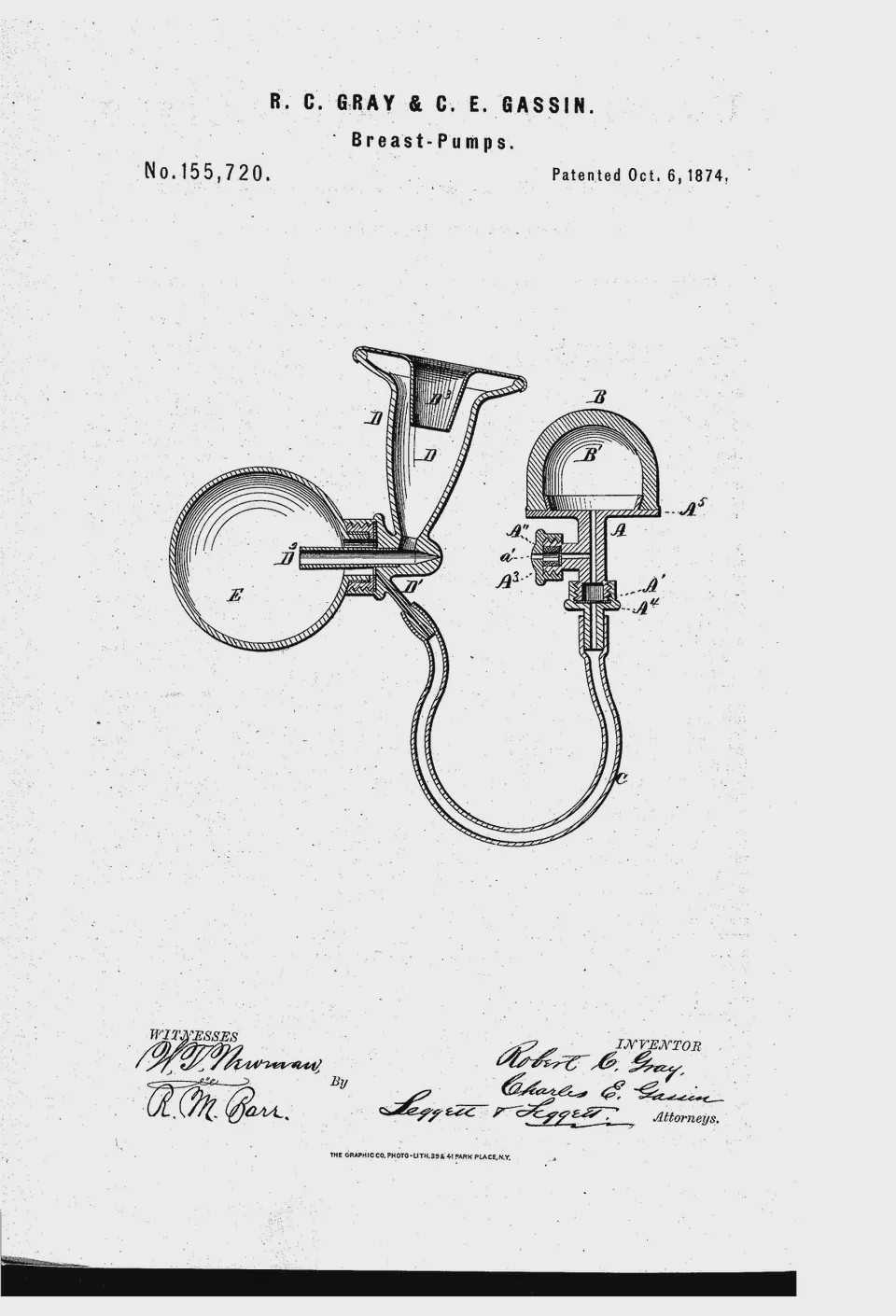 Still looks pretty scary to use ?
Still looks pretty scary to use ?
Now, here?s a thought-exercise: would you ask an interior designer to do your taxes? A taxi driver to file your divorce? A therapist to do your brain surgery?
Many products weren?t built with women in mind. It hasn?t just been breast pumps. Medical devices, period products and bras are just a few more examples.
?????
We valued milking cows more than milking women in 1854. Luckily, we have fancier breast pumps today. Along with more women?s rights, contraceptives and openness about ?taboo? topics. We?re doing a lot better today than we were 100 years ago.
But that isn?t good enough.
There are still so many unsolved problems that only women experience.
?Periods are painful, messy and confusing.
?Pregnancy is emotional, difficult, and in some parts of the world, deadly.
?Menopause is uncomfortable, awkward and aching.
The ?developed? world still has a long way to go. Nevermind the developing world. 70% of the poorest 1B people are women.
?Women don?t have access to menstrual sanitation, contraceptives or safe abortion.
?Poor sexual education and medical infrastructure.
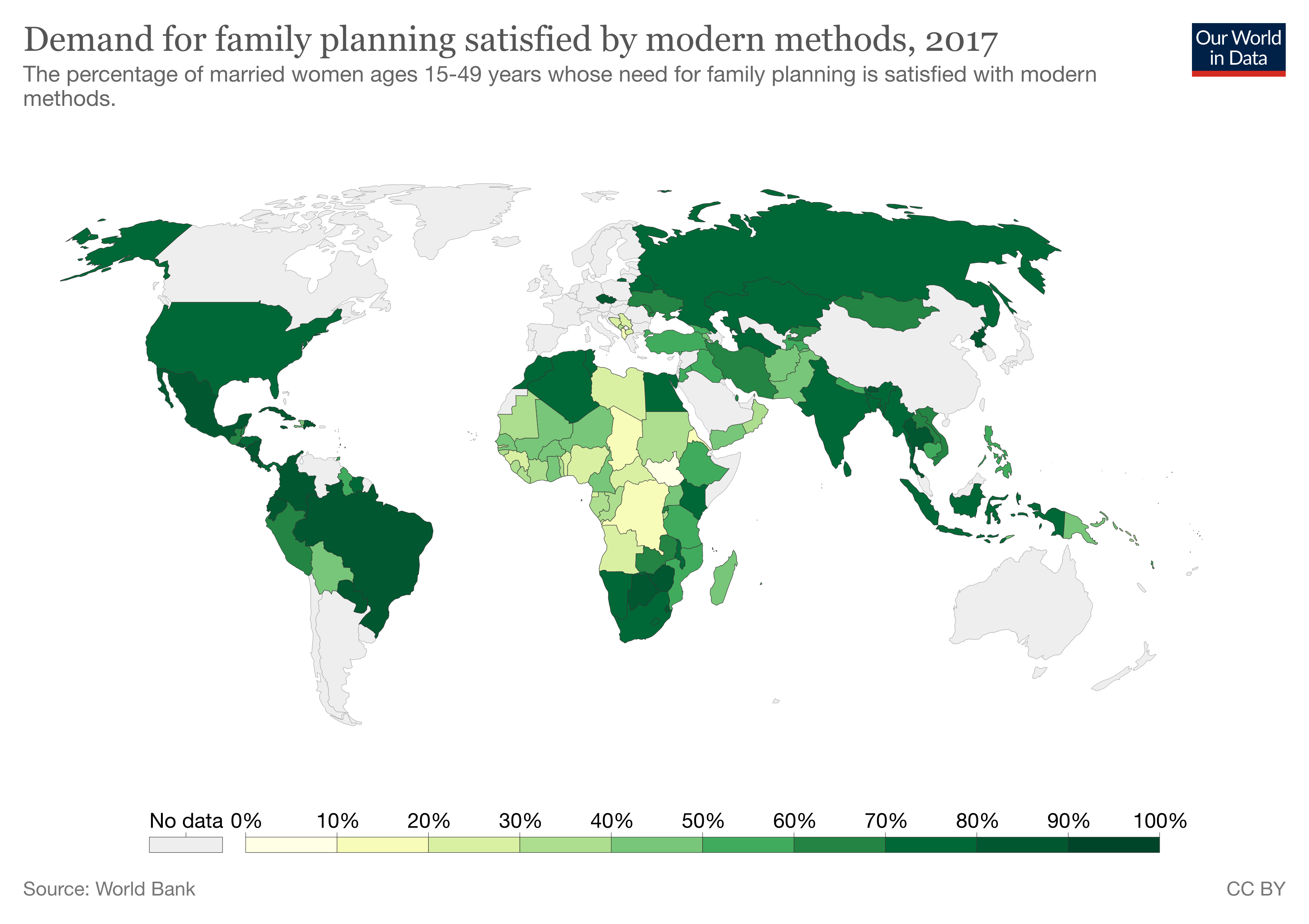
? There?s also an economic incentive behind helping women?s health. Nigeria, Senegal and Kenya could increase per-capita income by up to 65% if they met all contraceptive needs.

In this post, I?ll go over all areas of women?s health. You?ll leave this article understanding:
1 ? Each of the main ?phases? in a woman?s life, the main pain points and why they?re important. Specifically:
- Menstruation
- Contraception
- Conception
- Pregnancy
- Birth/Nursing
- Menopause
- Main Diseases
2 ? The concepts and areas that femtech can disrupt, and key plays in each field.
3 ? A lot of crazy statistics that should not exist.
Why should we care about women centred products?
For a long time ? most of history, we thought women and men had the same bodies. Only women had boobs and periods.
We?re learning that it?s not that simple. Women are very different than men. We need different products.
That?s what?s been driving the rise of ?femtech? (female technology). Products made for women.
I?m a nerd, and I like numbers.
What?s the state of the femtech industry?
Despite knowing men + women are very different, we aren?t investing in women?s health.
- We direct 4% of global health research towards women-specific studies
Men still dominate femtech.
- Of the 4 biggest funding rounds in Femtech, companies founded and built by men raised 3/4 rounds.
- 92% of partners at the biggest VCs are men; it?s hard to get funding for these companies. Imagine trying to explain a rocket science equation to a toddler; not impossible, but also not easy.
From an economic perspective, why is supporting women important?
They make household and hospital decisions.
- 83% of women have major buying power in their households
- 90% of women are primary healthcare decision-makers
Lack of women?s health investment costs the healthcare system lots of money.
- Women?s health has a $500B economic burden. In contrast, liver cancer has a $2.8B economic burden.
They reach for help more often and are willing to try new products.
- Women are 75% more likely to use digital tools for healthcare than men.
Now that you know some of the numbers, it?s time to get this party started! ?

Menstruation; period.
Once a month, girls go through their period. Sometimes this involved chocolates. Or cramps. Often there?s tears.
Most people, and alarmingly most women, don?t understand why this all happens.
I?ll give you a crash-course, but if you want the full details you can read my period article here.
First, it?s time to refresh on the female reproductive system.
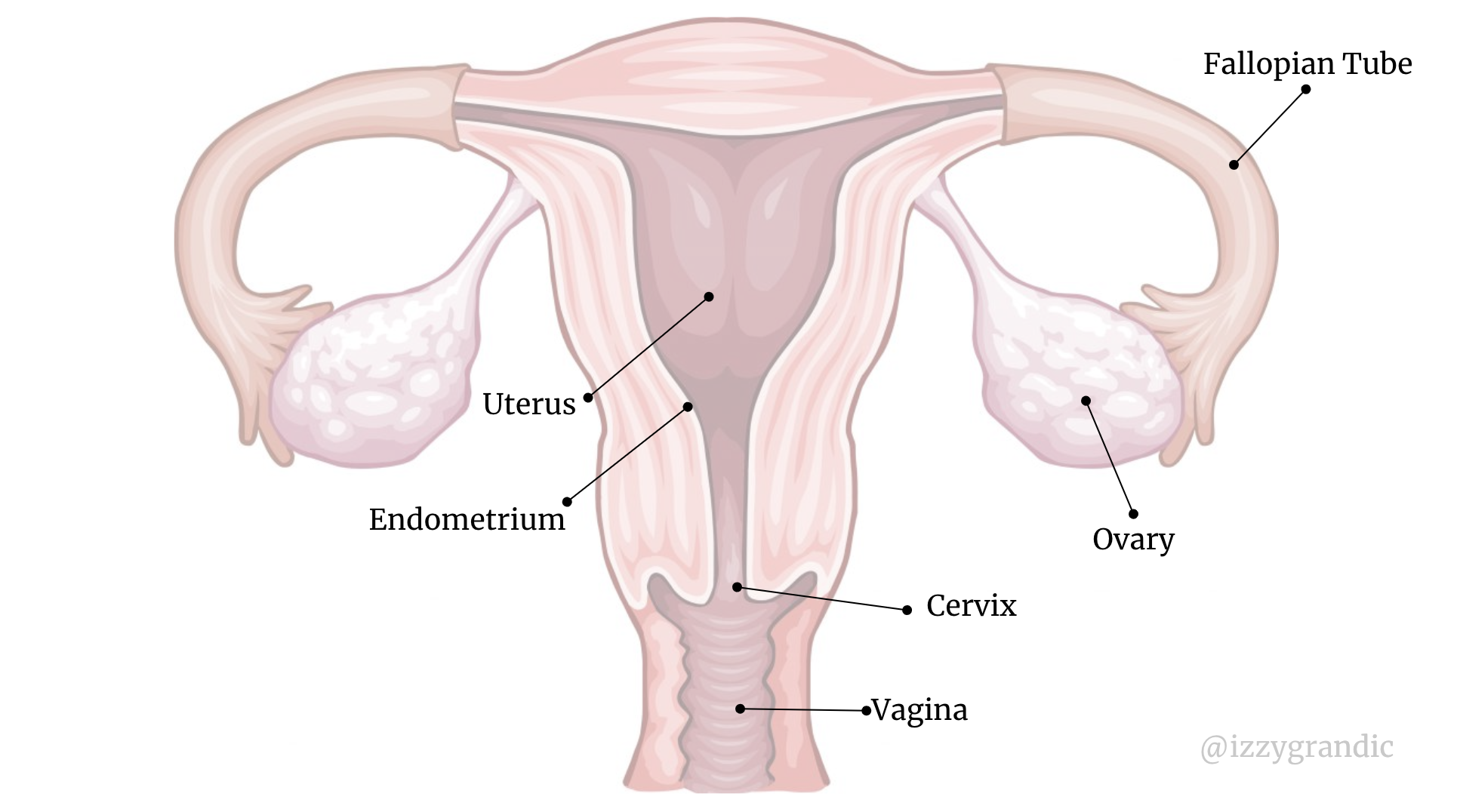
These are all the labels you need to know as you follow along.
Vagina = Entrance
Cervix = passage between uterus and vagina
Uterus = the womb
Endometrium = outer lining of the uterus, that sheds as the ?period?
Ovary = Matures and stores eggs
Fallopian Tube = Transports eggs into the uterus
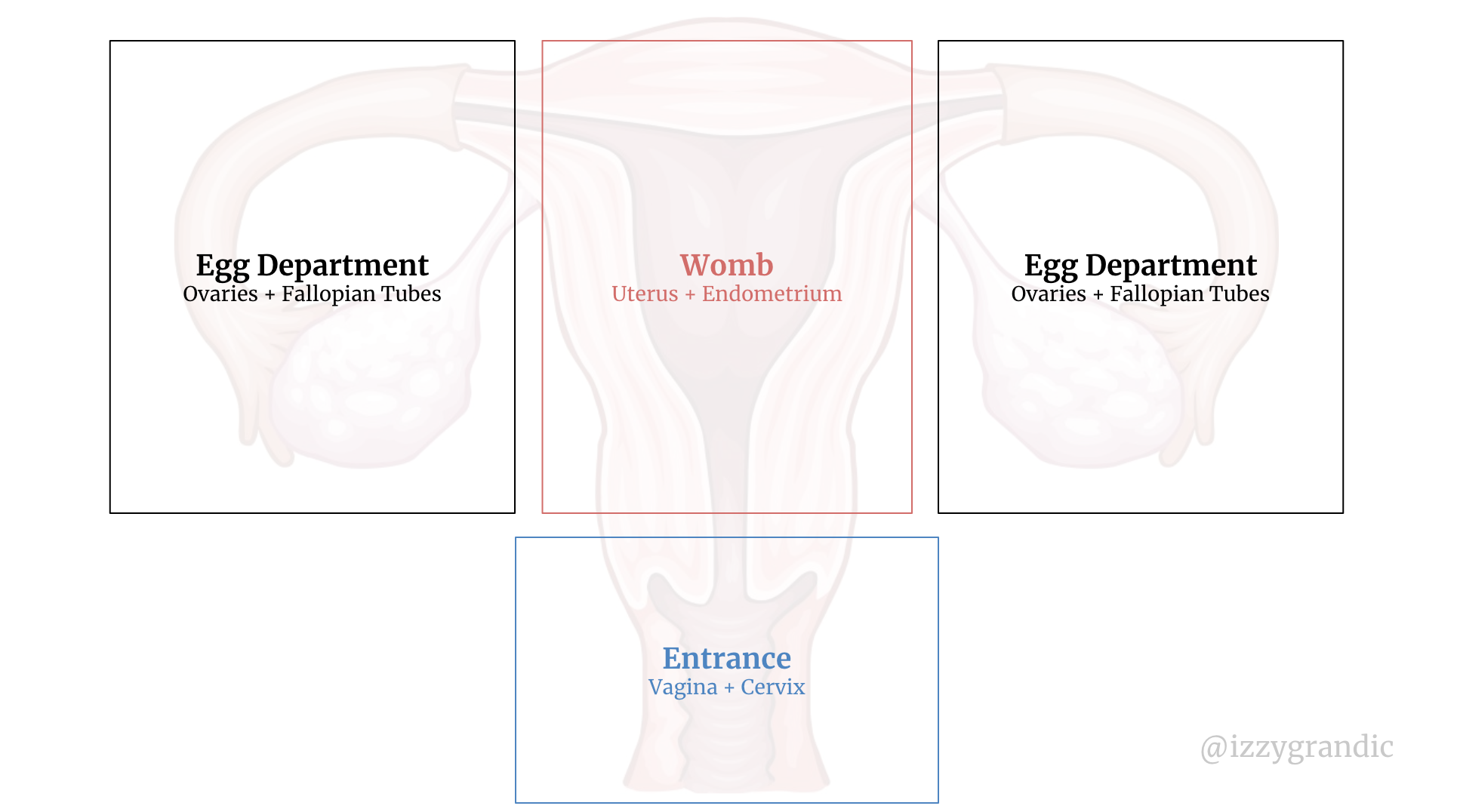
The female reproductive system has 3 different ?functions.?
- To let things in. This could be anything from sperm to tampons to medical devices.
- Make/transport/store eggs (sex cells).
- Womb: if a woman is pregnant, her baby will develop in there.
Here?s how the body organizes the departments:
Why do we get periods?
Women have eggs, and these eggs, combined with sperm, can make a baby. Women?s eggs rest in their ovaries.
- In the ovaries, 100s of immature egg follicles start to mature. After 7 days, we choose a ?dominant egg,? and the rest of the maturing follicles die. After ~14 days the dominant egg is fully mature.
- The dominant egg leaves the ovaries and enters the fallopian tubes on day 14. It waits here to meet a sperm. We call this ovulation.
- The woman?s body prepares for the potential situation that a sperm comes by. It thickens its muscular layer (the endometrium). It releases hormones and makes mucus.
- If a sperm comes by, the body is all set to develop the sperm-egg pair (called a zygote) into a baby. If a sperm doesn?t come by, the body destroys its thick muscular layer and discharges the egg. This layer contains many blood vessels, so when it exits the body, it looks like blood. That?s a period.
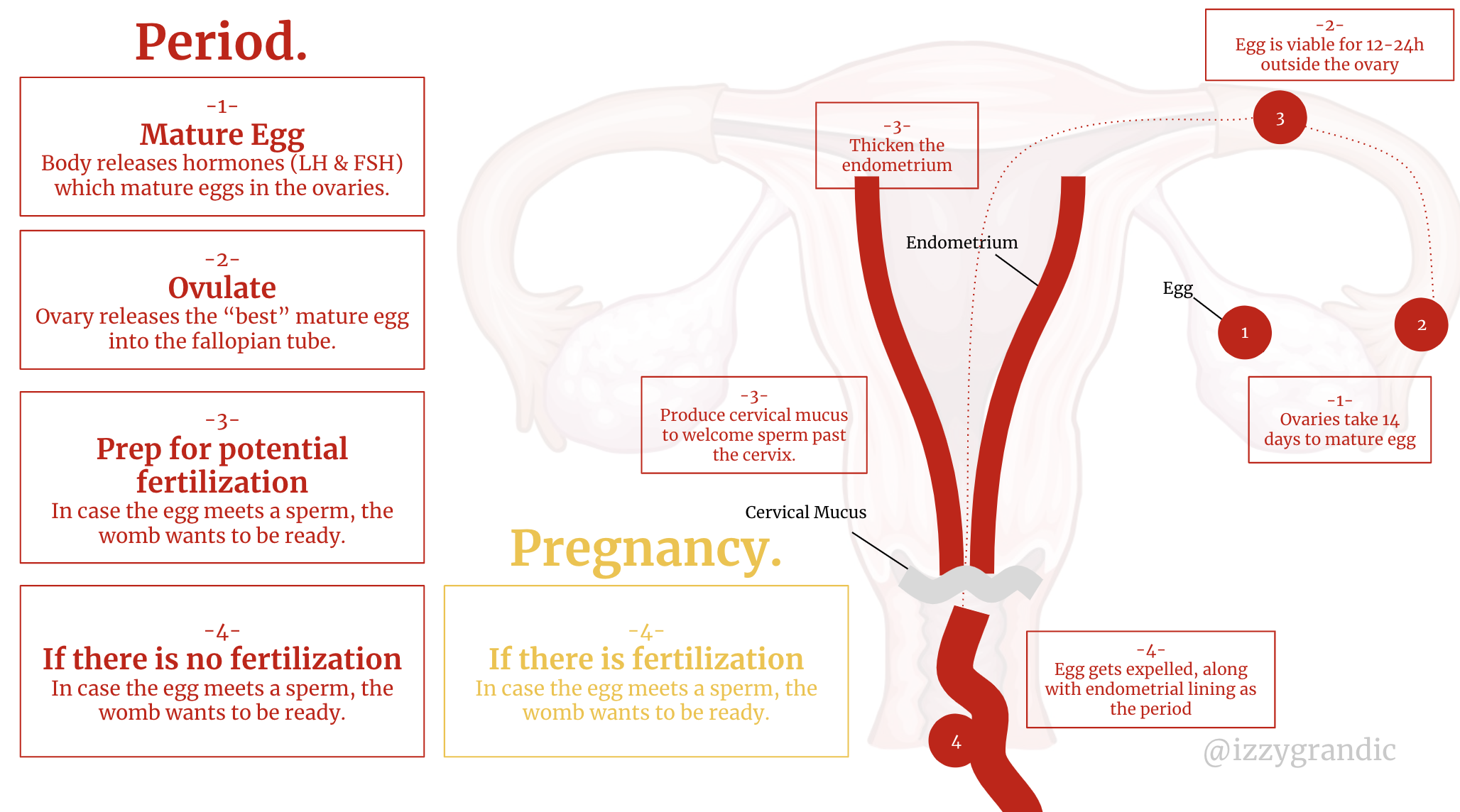
Menstruation is actually made up of two cycles:
- Ovarian: the process of releasing an egg (ovum) from the ovaries.
- Uterine: the process of preparing the uterus (?womb?) for a potential baby.
TLDR: we get periods when our body prepares for a baby, but our egg doesn?t find a spermy friend.
Periods change our lifestyle.
Women are clocks that are always changing (hormonally). They operate on a (~28 day) cycle. Each day of their cycle their body is in a different hormonal state.
For men, their bodies aren?t an every-changing hormonal clock.
So, doing things like eating the same thing every day, or working out the same every day is fine. They?re dealing with the same ?body? so it makes sense that they can do the same ?things? to it, whenever.
But one-day women might have a ton of estrogen ? and the next day it?s 30% lower. You can?t treat your body the same on these two days. Chemically, it?s not the same.
Women should be adjusting their schedules and routines to their bodies ? rhythms. I won?t give specific health advice, but here are a few resources to explore:
- Changing your diet based on your menstrual phases
- What to eat, according to your body?s phases
- How to exercise and eat
But the main implication is: if your body is changing, so should your lifestyle.
There?s a notion of women being ?unpredictable.? But, we?re actually very predictable, most external people don?t pay attention. We live on an ever-changing cycle. The more you understand about your cycle or the cycle of any female close to you, the smoother the lifestyle you?ll have.
But many people pass through life letting their body surprise them. That?s when constant lifestyle changes can become an issue.
Periods are wasteful.
In 3 years, women use ~700 pads or ~800 tampons.
They?re expensive, which leaves people in unsanitary conditions.
- 80% of adolescent girls in India are aware of sanitary napkins but only 30% have actually used them.
- 70% of women in India say their family can?t afford to buy sanitary napkins
- 88% of women in India do not use sanitary napkins often.
What do they use? Old rags, plastic bags & anything they can find. We call this period poverty and it impacts 500M women.
 Items people may use instead.
Items people may use instead.
Recapping the problems with periods
- Physically painful
- Emotionally painful
- They alter lifestyles, which can be confusing. Or, women don?t know that they should be adjusting their lifestyle.
- Wasteful
- Unsanitary
How does Femtech come to play?
Women menstruate for several decades, spending 7 years? worth of time on their period. For some, the experience is painless, for others, they can?t even walk during their period.
It varies. But it?s something we all go through at one level or another.
We can separate menstruation femtech products 3 categories:
- Collection methods
- Symptom tracking
- Solutions to any pain/disorders
Collection Methods
If we didn?t have period collection methods, the world around us would be a lot redder.
What are the methods that exist today?
There are only 2 types of methods to collect blood; each method has a range of products.
1 ? outside the vagina
Period blood exits the body through the vaginal canal. This type of collection collects after the blood leaves the body.
Things that fall under this category:
- The pad.
- Reusable Pads
- Pantyliners (thin versions of pads)
- Period Panties (underwear with a built-in reusable pad)

These are all like modified diapers. (Which isn?t a bad thing!)
They sit in your underwear (or are your underwear ?) and collect blood without leaking. Well? hopefully without leaking?
We?ve actually been using ?pad-like products? for a long time. But in the 1800s women used underwear made out of rubber or old rags stitched into panties.
 Or, the comfy hoosier belt.
Or, the comfy hoosier belt.
Non-reusable pads are actually more novel than reusable pads.
Your period blood passes through your vagina, which is a cozy home for bacteria. The blood contains microorganisms, tissues, vaginal mucus and other fluids. TLDR: It?s not the cleanliest activity to sit in a pad for 12h+ per day.
Not to mention, fecal bacteria are nearby, so they might hop over for the bacterial party.
Sanitation is the problem. The more you change your pads, the better. This is especially an issue for re-usable pads. If they?re not washed properly, you?ll be sitting in bacteria for days.
Sitting in one?s fluids can lead to infections and vaginal discomfort.
If a woman is not careful, she may end up with Bacterial Vaginosis. It?s a funny word and makes me chuckle a bit, but it is not a fun experience.
This is less of a problem in the western world with washing machines and access to cheap disposable pads. But it?s a major concern for the developing world.
- Many people who can?t afford products make their own DIY reusable pads using old rags or clothing.
- If they can?t afford a 10 cent panty napkin, it?s gonna be a lot harder to buy a washing machine. Over time, these rags will get stained with blood/unclean to use because of poor washing.
2 ? inside the vagina
Why sit in your blood all day, when you can proactively collect it, with no leaks?
Things that fall under this category:
- Tampons (disposable)
- Sponges (reusable sponge that soaks blood)
- Diva Cups (reusable cup where you can collect blood)
- Menstrual Disc (disposable alternative to diva cups; provide more comfort than tampons)

These products have a reputation for being scary. It?s easy to visualize how sticking something ?up there? can be frightening.
We?ve technically been using tampon-like-products for a while now. In ancient Greece, women would wrap lint around a hunk of wood. Not surprisingly? that didn?t stay in style. Over time, pads gained more popularity and we stopped shoving tree pieces up our vaginas.
In the late 1920s, doctors started getting more and more concerned with the hygiene of pads. In 1928 Alexander Flemming discovered penicillin, which lead to antibiotics. There was a hype around anti-infection products.
In 1933, Dr. Earle Haas patented and invented the modern-day tampon. And, in general, we haven?t made many changes to its design.
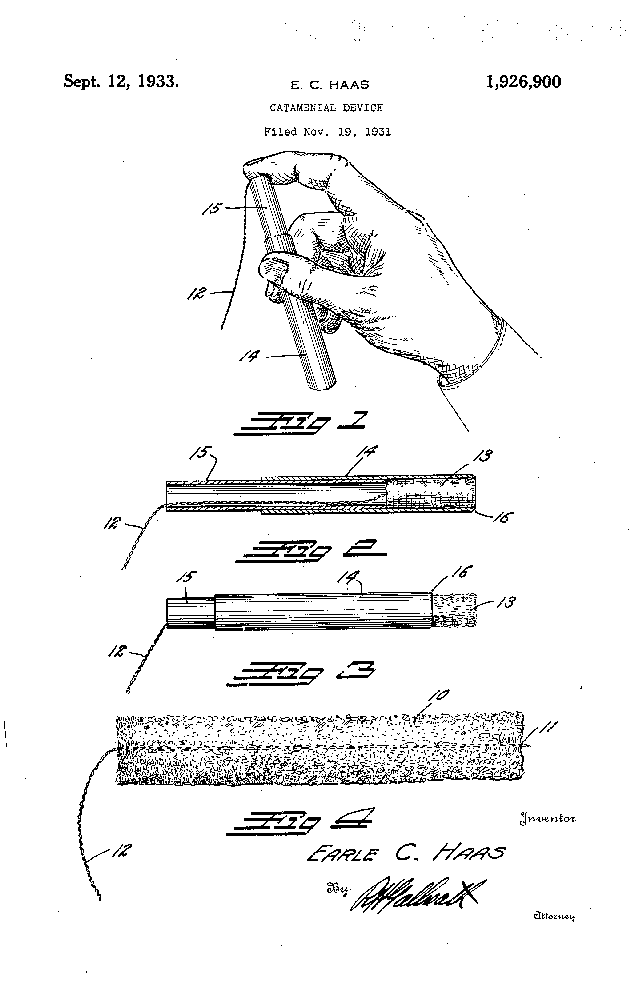 The modern tampon patent.
The modern tampon patent.
What are the downsides to inner vagina period protection?
Moral Dilemmas: several cultures/practices and people around the world are uncomfortable with the idea of tampons. Some say they ?take away virginity.? Other concerns surround women touching themselves. There?s varying opinions on the use of tampons, but often, it?s a sticky subject.
Toxic Shock Syndrome (TSS): caused by the overgrowth of bacteria Staphylococcus aureus. Tampons do change the bacterial structure of vaginas. But, they?re generally viewed as more sanitary than pads.
In the 70s, Proctor & Gamble introduced a product called ?Rely.? It captured 25% of the booming tampon industry because it was a single tampon you could wear for your whole period. Sounds good in theory, not in practice. These tampons were too absorbent, which caused TSS. Today, best practices are keeping your tampons in for <8h.
Well, now you?re a collection method pro! How are we changing the way we collect period blood?
Within the collection market, I?m seeing a few key trends:
- Focus on organic/wellness marketplaces, because tampons have weird chemicals.
- Tapping into smart products, to improve data collection.
- More sustainable options (e.g., reusable underwear, better versions of diva cups) Menstrual products like pads and tampons are the fifth most-common waste found on beaches
What I?m not seeing:
- A heavy emphasis on affordability. We?re leaving many girls in the developing world/rural areas behind. ?Organic? tampons are more expensive. Reusable options often require washing machines for effective use.
Symptom Tracking
What can we track?
- Tender breasts
- Bloating, fluid retention
- Muscle aches
- Joint pain
- Headaches: 1.7x ? 2.5 more likely to get them leading up to/on your period.
- Acne: 50% of women will notice an increase of acne a week before their period.
- Abdominal cramps: 80% of women can relate.
- Diarrhea or constipation
- Lower back pain
- Trouble sleeping
- Low energy, fatigue
Note: most of these symptoms occur due to the rising and falling of hormones. For example, progesterone causes breasts to enlarge their milk glands. This leads to breast enlargement, swelling, and well? milk.
Before menstruating, girls go through a process called ?PMS,? (or pre-menstrual syndrome). Each woman has a different PMS experience (which lasts ~3 days).
PMS affects women in two main ways:
- Physical changes: bowel movement patterns, breast tenderness, cramps, etc.
- Mental changes: the cocktail of hormones can cause crying spells, anxiety, anger, etc.
Some women have very severe versions of PMS that last much longer (7?10 days vs a few days). We call this Premenstrual dysphoric disorder (PMDD).
30?40% of the time, PMS symptoms are so severe they impact normal day-to-day function.
 PMS in a nutshell.
PMS in a nutshell.
Why is symptom tracking is important?
1. With pattern recognition, you can take appropriate action. Symptom tracking is about understanding your body so you can recognize patterns.
Let?s take PMS as an example. You can?t ?diagnose? it without keeping track of your symptoms. PMS for each person varies. Once you know what causes your PMS, your doctor can help identify patterns and treat the underlying causes.
2. The more you understand your body, the faster you can detect problems. When your cycle or symptoms become irregular, that?s a sign of imbalance. I can barely remember what I ate 3 hours ago, nevermind the exact symptoms I experienced 3 weeks ago.
3. Women?s health-related symptoms are similar. It can be hard to tell the difference between pregnancy and PMS.
Hormonal imbalance tends to result in similar symptoms. (Any of the mentioned above are examples). Keeping a detailed diary can help your doctor prescribe the right treatment.
4. You get less ?surprised.? Before I started tracking my period, every month I?d have it surprise me, at what felt like, all the worst times. When you track your cycle, you stain less underwear, and you?re always prepared.
What it all boils down to is: monitoring health, and staying in control of your cycle.
And here?s the good news: there?s definitely an app for all your period tracking needs.
Now you?re all caught up on the symptoms. Why do they happen? Hormones. Hormones. Hormones.
? but that?s as far as our answer goes. We don?t know how hormones do it, just that they do.
What?s the next wave of symptom tracking? There?s two aspects to it:
- Moving beyond manual input. Measuring & automating other metrics like mucus, blood, hormones (yay!), saliva, and sweat.
- Targeting specific niches. Building an app for 30-year-old women trying to get pregnant, is different than for teenage girls in Somalia. There?s a lot of potential to target underserved groups of girls!
More and more women are getting hooked into period-symptom tracking. We have 100s of apps out there. But, we still have so much to learn about symptoms and especially hormones.
Pain/Disorder Solutions
We talked a bit about diseases/problems with women ?down there.? If you want to go deeper, I wrote about female reproductive conditions here and here.
Types of menstrual disorder:
A disorder is when a woman experiences abnormal menstrual activity.
- Amenorrhea: the absence of bleeding
- Oligomenorrhea: Light or infrequent menstruation
- Abnormal Uterine Bleeding: bleeding at times other than your menstrual cycle.
- Menorrhagia: abnormally heavy or prolonged periods.
- Endometriosis: internal bleeding
What causes these disorders?
Like most diseases, it?s difficult to pinpoint their exact cause. But, often it?s a strange disease that causes it.
Think of your ?normal? period like a strawberry/banana smoothie. If you add a pound of nuts in there, it?ll be a little chunky and difficult to blend. If you add a gallon of water, it?ll be way runnier. When we change the physical environment of our reproductive system, we change its functionality.
Let?s talk about the nuts and water our bodies add to our smoothie:
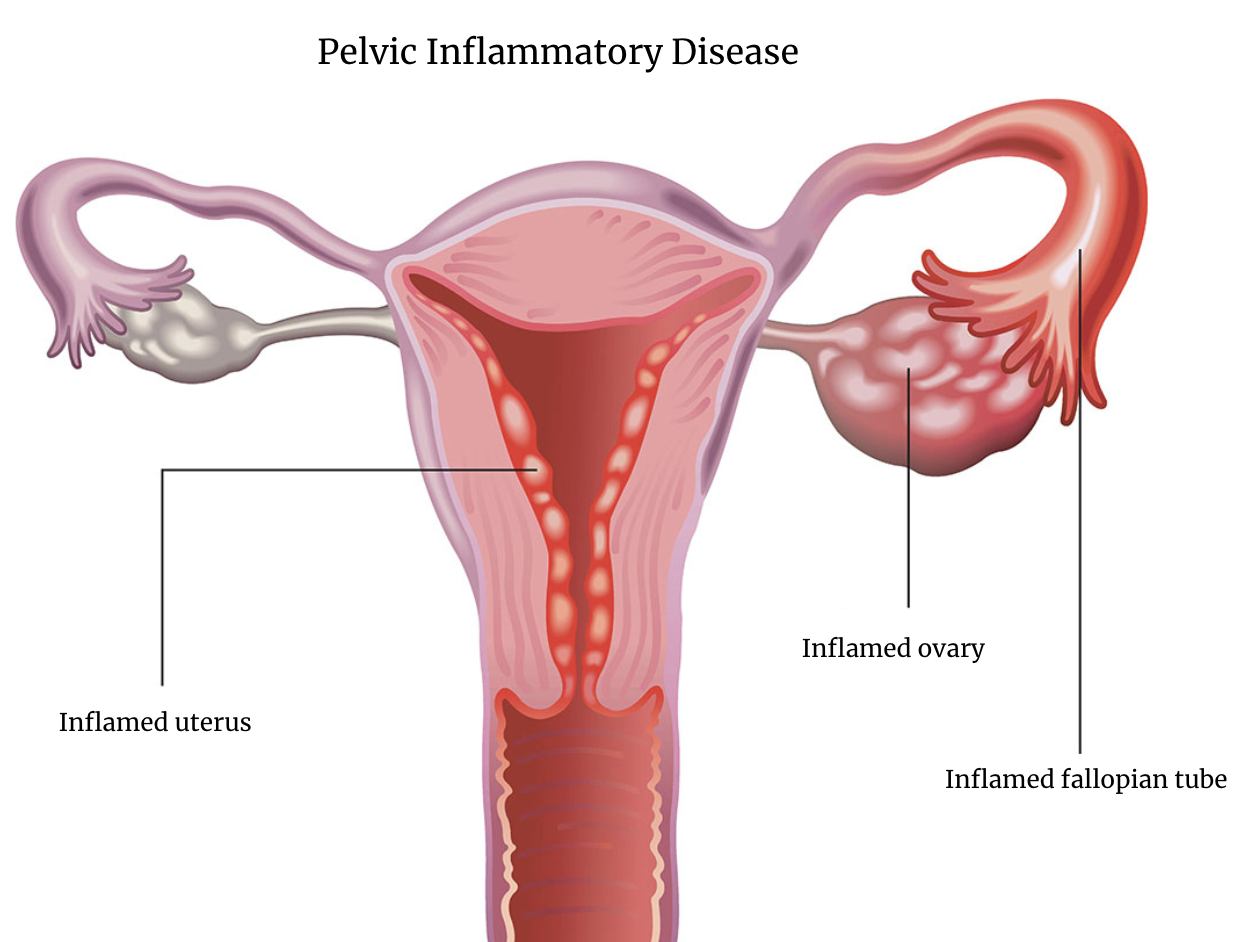
- Pelvic inflammatory disease (PID): inflammation of your pelvic area.
- Uterine fibroids: cancer-free tumours that build up in the uterus.
- Infection, tumours, or polyps in the pelvic cavity.
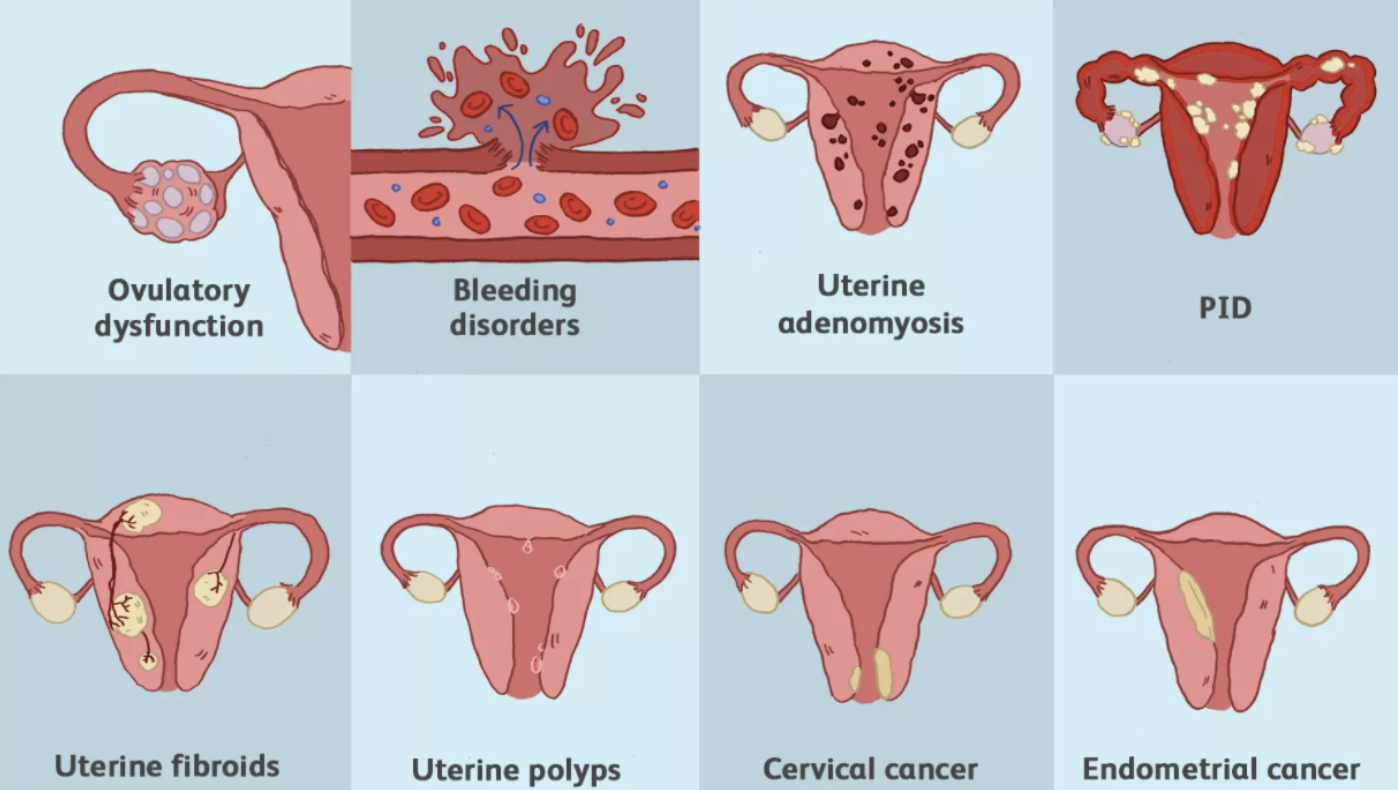
For a more in-depth description of these diseases, I would recommend this reading.
Periods should be a vital sign. We find these problems too late.
Picture this: you?re in severe back pain. You got to your doctor. They ask about your recent experiences and measure your vitals. And then, they ask ? oh, by the way, how?s your period??
It feels random and unrelated for your doctor to ask for such ?personal? information. But why? It?s not like your heart-rate, or weight directly correlates to your back problem. These are ways to measure how healthy you are.
But, our doctors don?t ask. And we rarely question our menstrual health.
We check up on our cars more than we check up on our uteruses!
Here?s the other problem: when we identify an issue, there?s very few things we can do about it.
After getting diagnosed, your options are normally: some surgery, medication or a lifestyle revamp.
How can femtech improve this system:
- Better imaging. Prevent things before they get worse.
- Better symptom tracking. This will help people recognize abnormalities sooner.
- More research into solutions. Endometriosis and polycystic ovary syndrome (PCOS) are still being treated with hormonal interventions introduced more than 50 years ago.
Contraception
With menstruation, comes the ability to get pregnant. Many sexually active women don?t want little versions of themselves running around them (yet).
That?s where contraceptions come in. They give people the ability to have baby-free sex.
?Some stats
- 99% of women in the US have used contraception, in one form or another.
- Women spend 30 years using contraceptives.
- For every $1 invested in family planning, governments save $7.09.
Contraception changed the western world.
More degrees: college enrollment increases by 20% when women have access to the pill. And, their dropout rate is 35% lower. # of women who complete 4+ years of college is 6x higher when birth control pills are legal.
Less teen pregnancy: figures have dropped by 51%. , birth control handles 86% of that decrease.
Less unintended pregnancies: it?s illegal to get an abortion in many countries. That leaves women in a situation to get illegal or dangerous abortions. Less unintended pregnancies = fewer abortions.
More Women in leadership positions: before contraception, no women was the CEO of a Fortune 500 companies. Now we?re at 5%, not great, but better than 0%.
TLDR: the pill gave women control of their fertility, which gave them control of their lives.
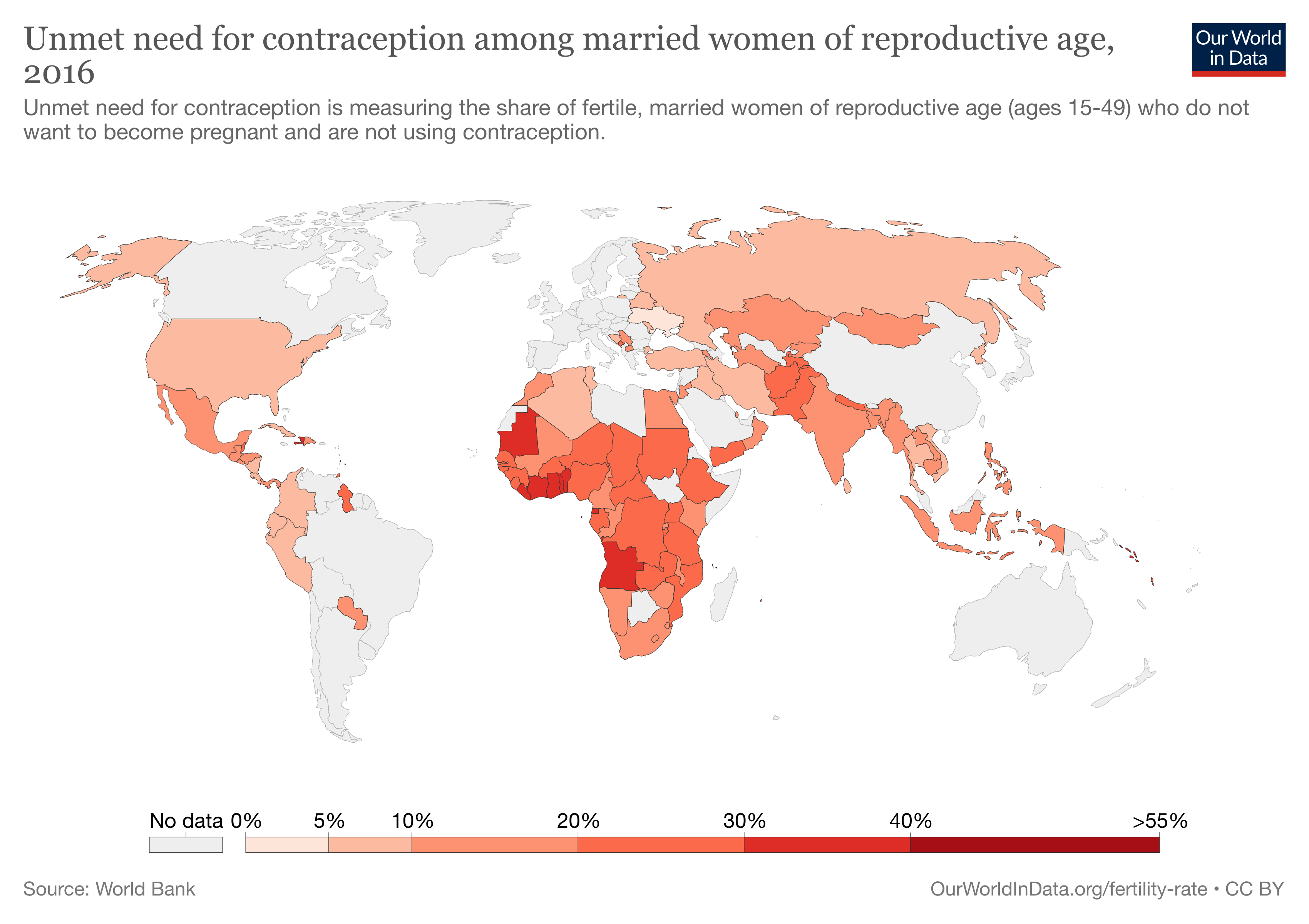
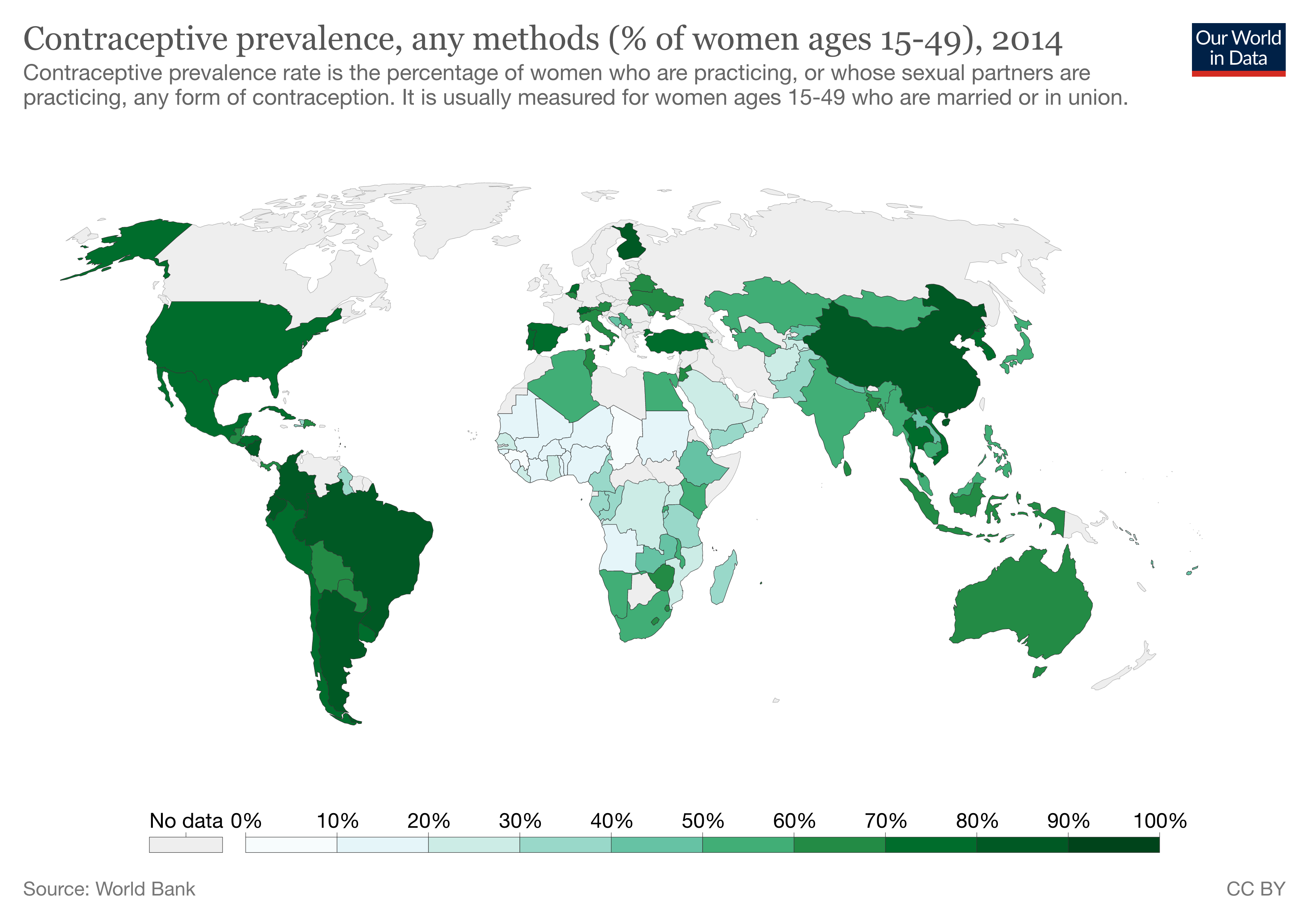
But, This isn?t the case everywhere.
In developing countries, especially in Africa, women lack access to cheap contraceptives.
The goal of contraception is to ensure the sperm and egg don?t make a baby in the uterus.
To avoid this, we can do one of a few things:
- Stop the sperm from entering in the first place
- Kill the sperm or egg
- Damage the endometrial lining; if the sperm/egg meet, they need to implant in the endometrium; if it?s damaged, there can?t implant, which kills the potential fetus.
- Time sexual intercourse such that the egg and sperm have no chance of meeting.
No method of contraception is 100% protective, but many come pretty damn close. Sometimes, women/couples use several forms of contraceptives to play it safe.
There are two ?classes? of contraceptives: normal and emergency.
Within these, we can split their methods into two categories: hormonal and non-hormonal.
Now let?s talk about safe sex ?.
What are the types of contraceptives?
Normal Contraceptives
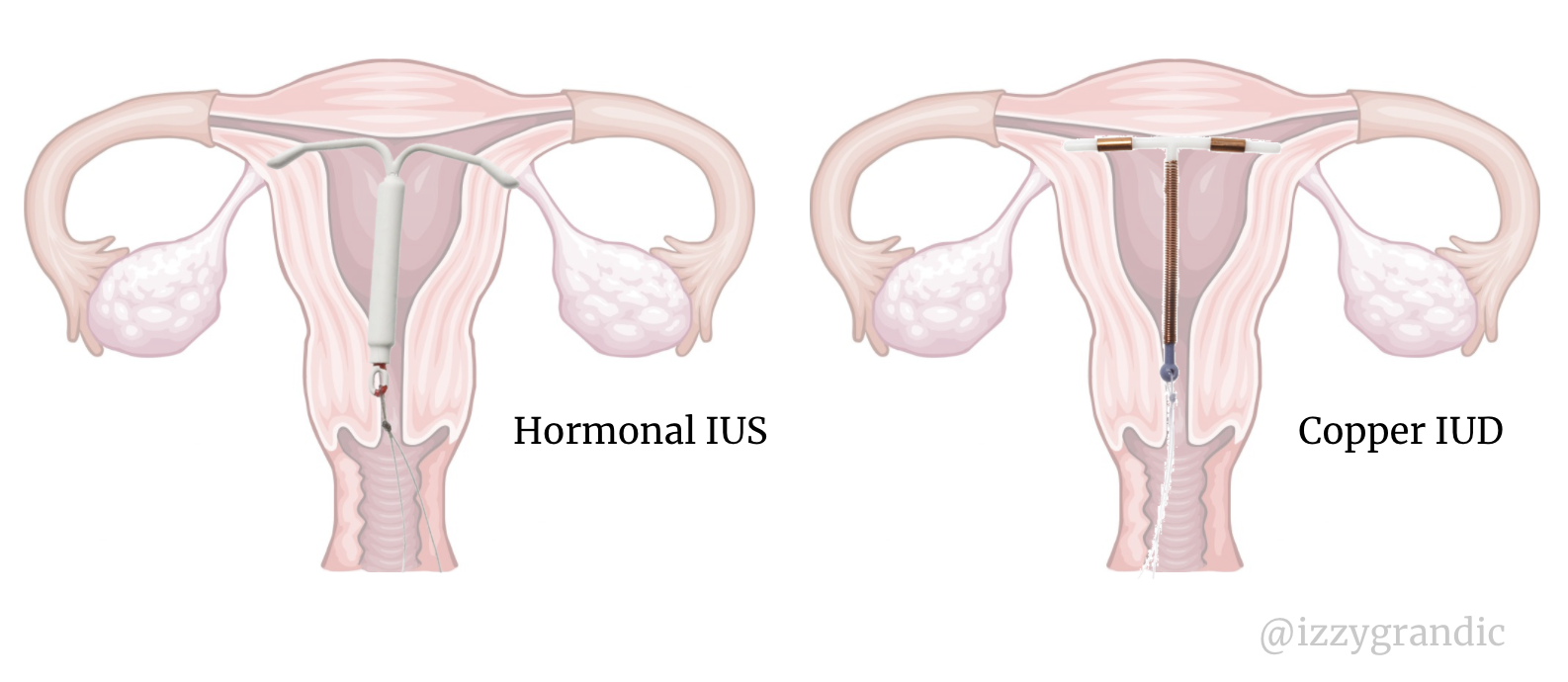
Intra-uterine contraception
?Intra? means ?inner,? and ?uterine? refers to the ?uterus.?
This type of contraception goes inside a woman and lasts 3,5 or 10 years at a 99% efficiency rate.
Once removed, fertility returns back to normal in a matter of days.
There are two types:
- Hormonal inter-uterine system (IUS): releases progesterone. This thins the lining of the endometrium. It also creates a ?cervical plug? which stops sperm from entering the cervix.
- Copper inter-uterine device: copper (metal) kills sperm and eggs.
Arm Implants (Nexoplan Birth Control)
This type of birth control is an implant inserted in one?s upper arm. It releases similar hormones to hormonal IUS. It lasts ~3 years.
 The small rod is surgically implanted into the arm.
The small rod is surgically implanted into the arm.
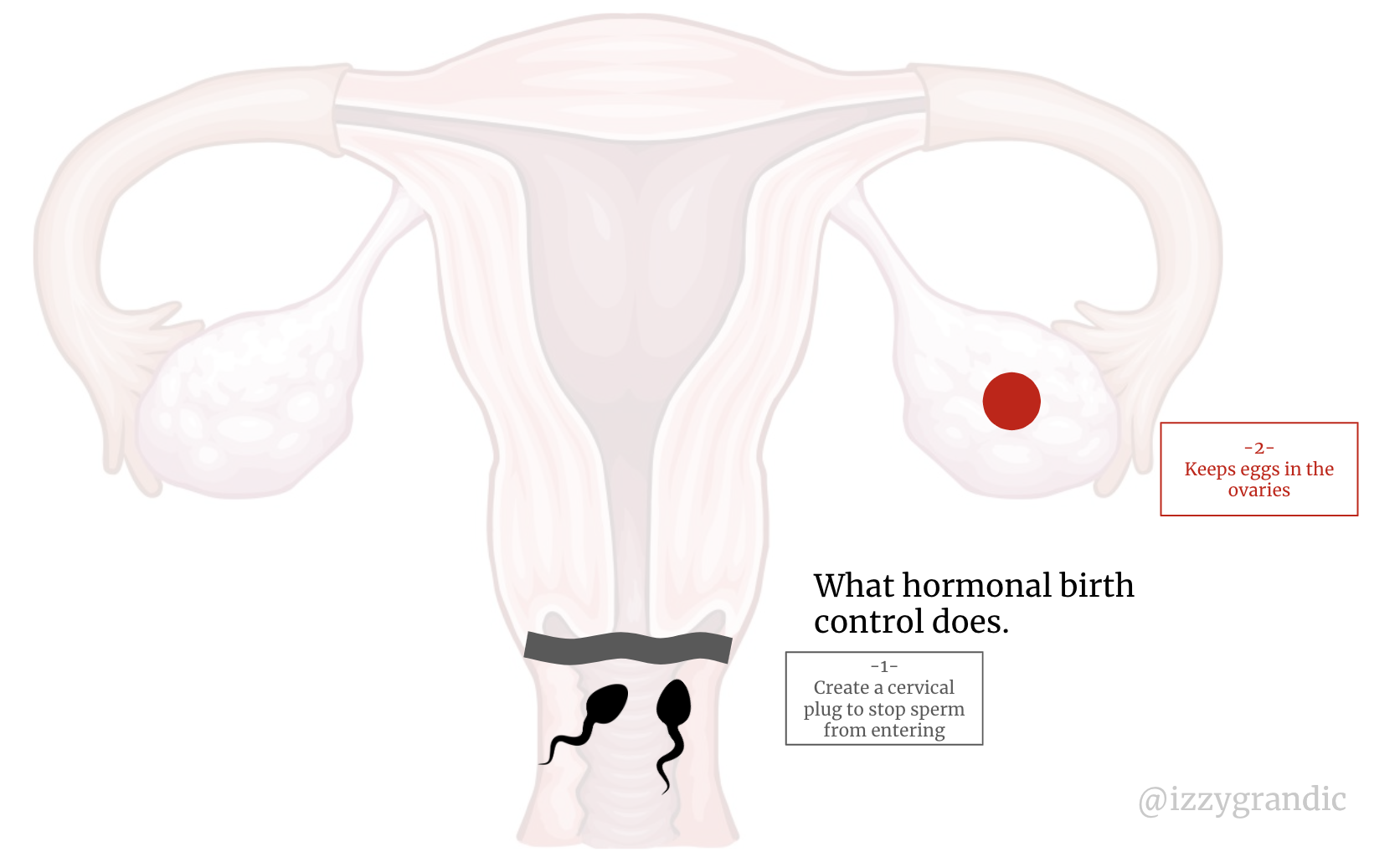
The Pill, Ring, Patch and Injectables
These methods release a cocktail of estrogen and progesterone to suppress the egg and create thick mucus to block the sperm from coming in.
 Adding more hormones to your body helps your egg disappear after ovulation.
Adding more hormones to your body helps your egg disappear after ovulation.
Each month, the female body releases 1 egg. If this egg disappears, there?s nothing for the (sometimes 100s) of sperm to mate with.
 *Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
*Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
There are two main types of this contraception:
- Combo pill ? contain estrogen and progestin (synthetic progesterone)
- Mini pill ? contain only progestin (designed for women sensitive to estrogen)
This doesn?t come free of side effects. The pill affects periods, nausea, mental health and more.
Diaphragm + Spermicide
Stops the sperm from entering.
Diaphram = physical blockage.
Spermicide = Set of chemicals that disables/immobilize/destroys the sperm. We can find spermicides in many forms like foam, cream and translucent films.
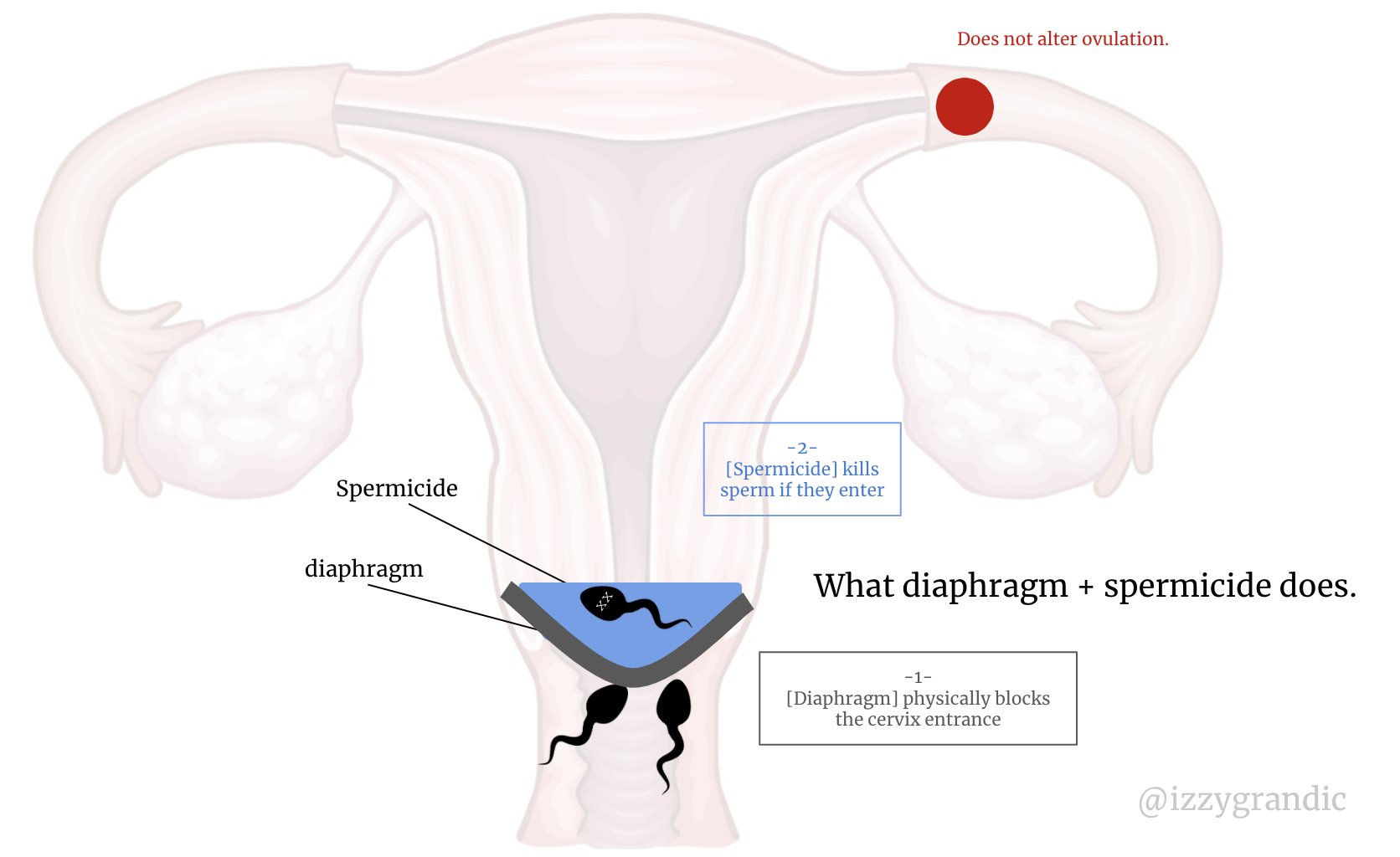 *Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
*Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
Condoms
I approached sex-ed class in high school with the same enthusiasm I have when my flight gets delayed 5h.
But, when my teacher pulled out the banana?
Condoms cover the penis, which stops the sperm from entering the vagina. That is a sentence I never thought I?d type to share on the internet.
Basal Body Temperature (?natural? birth control)
Since women are always on a ?cycle,? there are times of the month where their egg isn?t floating around. If it isn?t floating around, no sperm can mate with it.
?Temperature? is an indicator of what time of the month it is.
If women track their symptoms (?), they can avoid having sex when their egg is out-and-about. This is sometimes called digital birth control.
Emergency contraceptives
1 in 9 women has used an emergency contraceptive.
Morning-after pill (Plan B)
This pill has similar hormones one would find in birth-control, only at a much higher dosage.
It does 2 things:
- Prevents egg from fertilizing (doesn?t leave its ovary)
- Makes more cervical mucus to prevent sperm from reaching the egg.
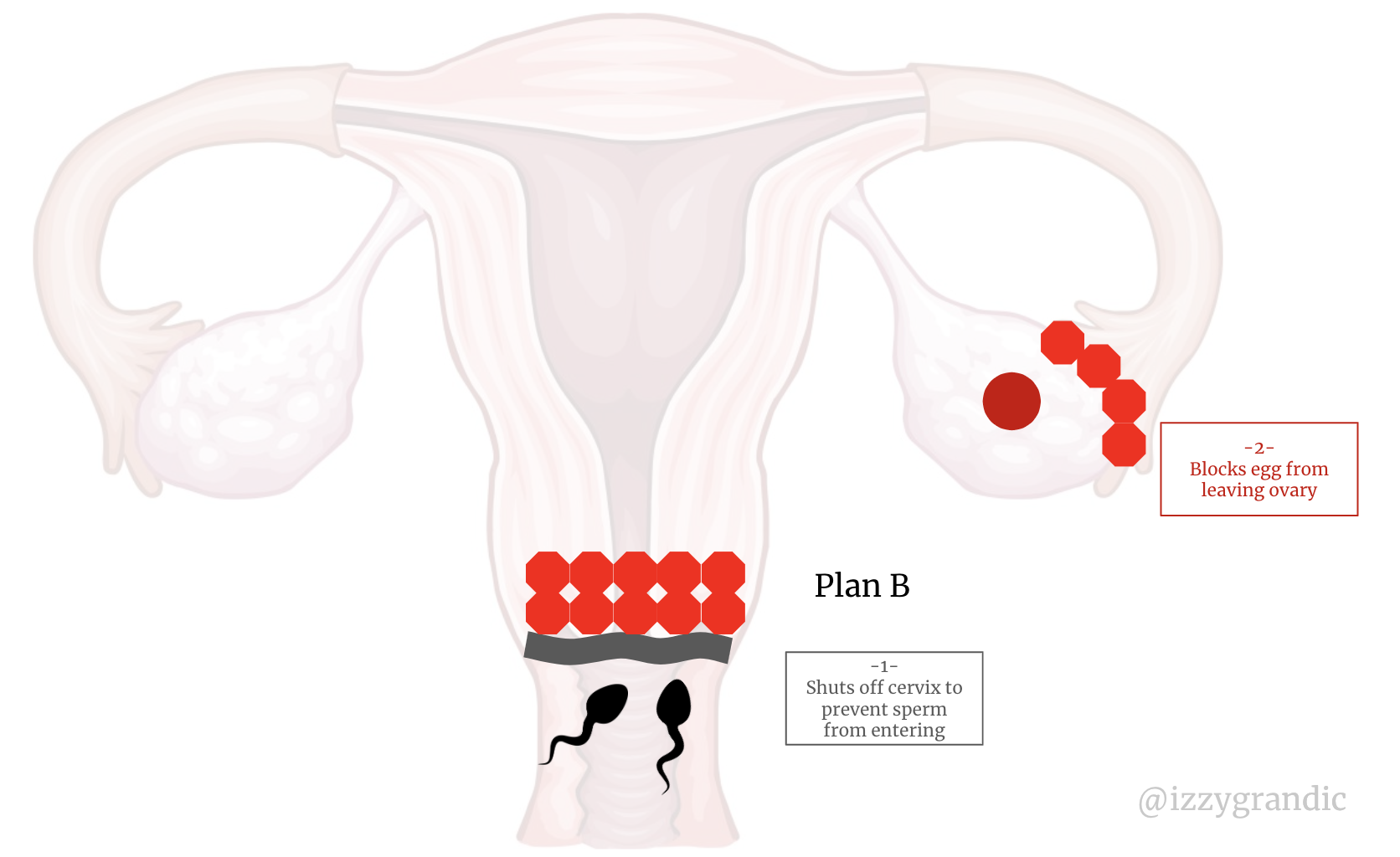 *Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
*Sperm magnified for the sake of drawing; they?re actually 30X smaller than the egg.
Nonhormonal Copper IUDs
We talked about IUDs above; we can use them for long-term contraception (last 3?10 years), or as emergency contraception.
They?re effective immediately when they?re inserted.
What?s the femtech opportunity here?
1-Choosing Contraceptives.
As you can tell, there?s lots of options. Yet, 41% of General Practitioners don?t do a proper risk assessment for contraceptives. Women might be taking the wrong dose of hormones, or dealing with avoidable side effects.
Where are the contraceptive algorithms at?!
2-Non-hormonal Contraception; or at least understanding hormonal contraception.
Right now, there?s an increased correlation with (hormonal) birth control and depression. I mean, we are injecting hormones, which do affect the brain.
Currently, we ask a few lifestyle questions to determine one?s type of birth control pill. It?s not targeted. There?s two things we should consider:
- Understanding how the hormones impact a specific woman?s biology. (Using algorithms, more testing, etc)
- Finding more alternatives. E.g., how to leverage our natural cycle, which is 98% effective with perfect use.
Conception
Here?s what they don?t tell you in health class: getting pregnant isn?t as easy as it seems. 1 in 7 UK couples experiences difficulty conceiving.
The goal of conception is the opposite of contraception: to get pregnant.
More and more people are waiting to have kids when they?re older, which also makes it harder for them to do so. The fertility market is booming! The IVF market (one alternative for infertile couples) will be worth $37.7B by 2027.
How does conception happen?
You?re about to embark on a journey to make a delicious waffle.
Specifically an eggo waffle with some spermy syrup (note: does not contain semen).
 Snack time!
Snack time!
The eggo waffle represents a woman?s egg; the spermy syrup is a male?s sperm. Together, eggo and syrup make a good snack. Together, sperm and eggs make a baby.
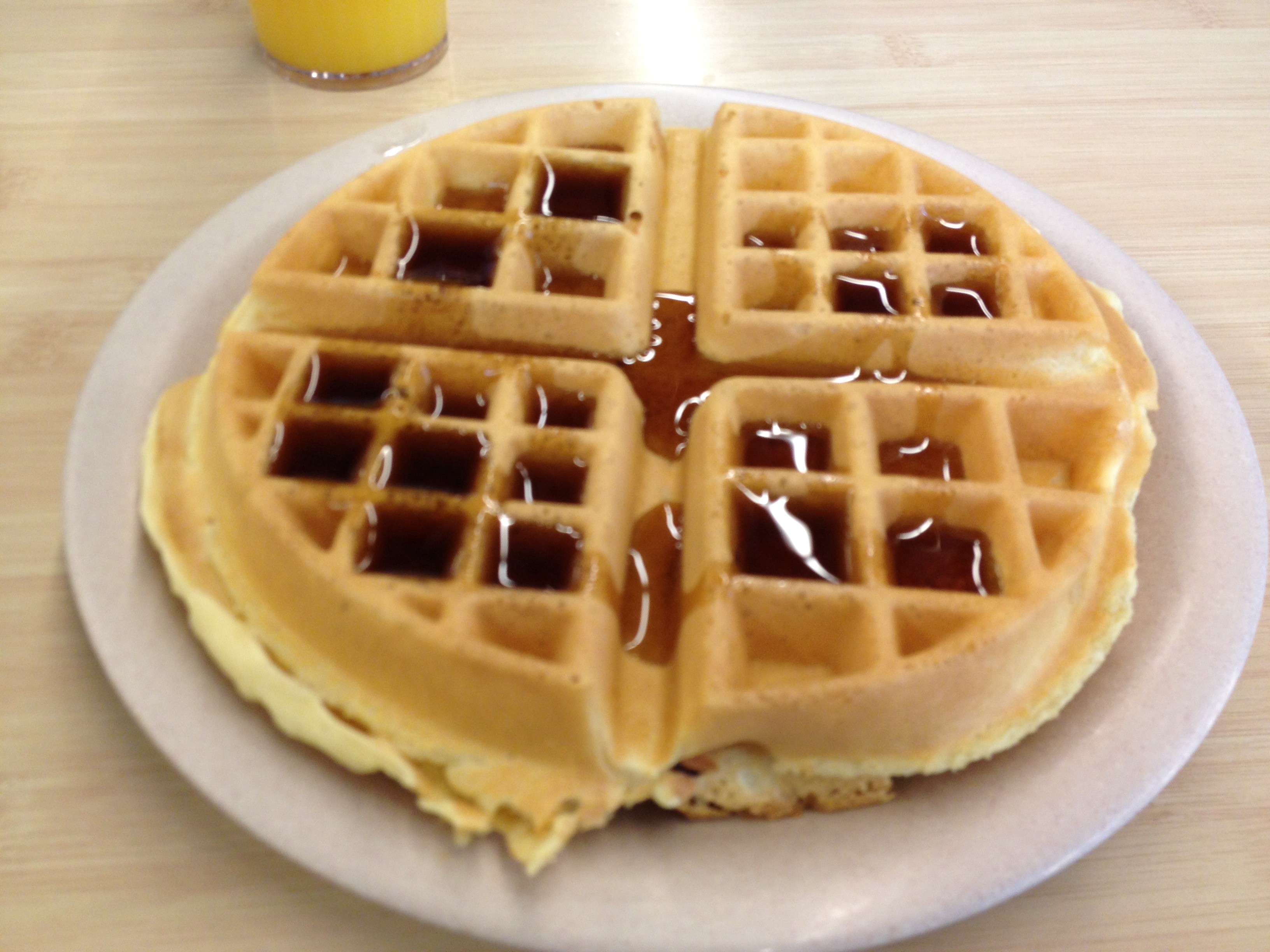
But, this isn?t a regular waffle making endeavour. Making that breakfast is not easy.
Here?s the deal: you?re a fitness guru and an eggo super-fan. To keep yourself motivated, you have a dedicated waffle room in your home. And you make this waffle extremely difficult to make.
The waffle room has a fridge with 999 bottles of normal syrup and 1 spermy syrup bottle. A freezer, with 1 eggo waffle. This singular eggo gets replenished once every 28 hours.
It?s a 3 story room. The first story has the fridge/freezer; the second is empty, and the third has your toaster. The stairs are spiral-y.

 It?s an adventure to get up!
It?s an adventure to get up!
Every 28 hours, you let yourself attempt to make a waffle only *if* you?ve been working out well. And you need to make it blindfolded.
To start the process, you grab the eggo from the freezer, and you go up two stories to get to the toaster.
You can put the eggo in the toaster for between 0?60 minutes (it?s a low-intensity toaster).
Here?s the (one of many) catch(s): the toaster randomizes its intensity. So, sometimes it burns the eggo faster/slower. Sometimes the eggo will last up to 60 minutes, sometimes it?ll burn to a crisp at 42. The less time in the toaster the better.
After placing the egg in the toaster, you go downstairs, grab a bottle of syrup, run upstairs to the toaster floor and taste it.
If it is the spermy syrup, you take the waffle out of the toaster. If it isn?t burnt, you place the syrup on top and enjoy.
There?s a 1/1000 of spermy syrup, so most of the time you need to run downstairs and repeat the process.
If you don?t grab the spermy syrup before the eggo burns; you?re out of luck. No waffle.
It?s a game of luck, not trying to fall down the stairs and perseverance.
With this process, within 14 days, you have an 85% chance of making 1 waffle.
Ah, the things we do to stay motivated to work out ?????.
This is conception.
- It?s an intensive journey to get the eggo waffle and spermy syrup together. When they do come together they?re ?fertilized? and ?implanted? into your digestive system.
- It?s time-sensitive (you have a short toaster window), and unpredictable (you don?t know when it?ll burn).
- You?re blind the whole time.
- Stress makes it worse. If you?re stressed, you?ll slow down. To do this process right, you need to be 100% committed.
- TLDR: it?s hard to make a baby.
Without using food to explain, what happens?
- Once a month, the female body releases an egg into one of her fallopian tubes. [Note: sometimes two eggs get released; if sperm fertilize both, then we have fraternal twins]
- When couples have sex, sperm can enter the vagina. ~300M sperm enter. Then, they go into the cervix; about ~100k make it through. This is the start of the sperm?s 6-inch-journey.
- Most sperm will get lost in the uterus and die. RIP. Some will go in the wrong tube. About 200 reach the egg.
- The 200 Sperm digg into the egg?s outer cell layer. The first one to make it all the way in fertilizes that egg.
- During fertilization, the egg and sperm combine their genetic material. They make a zygote.
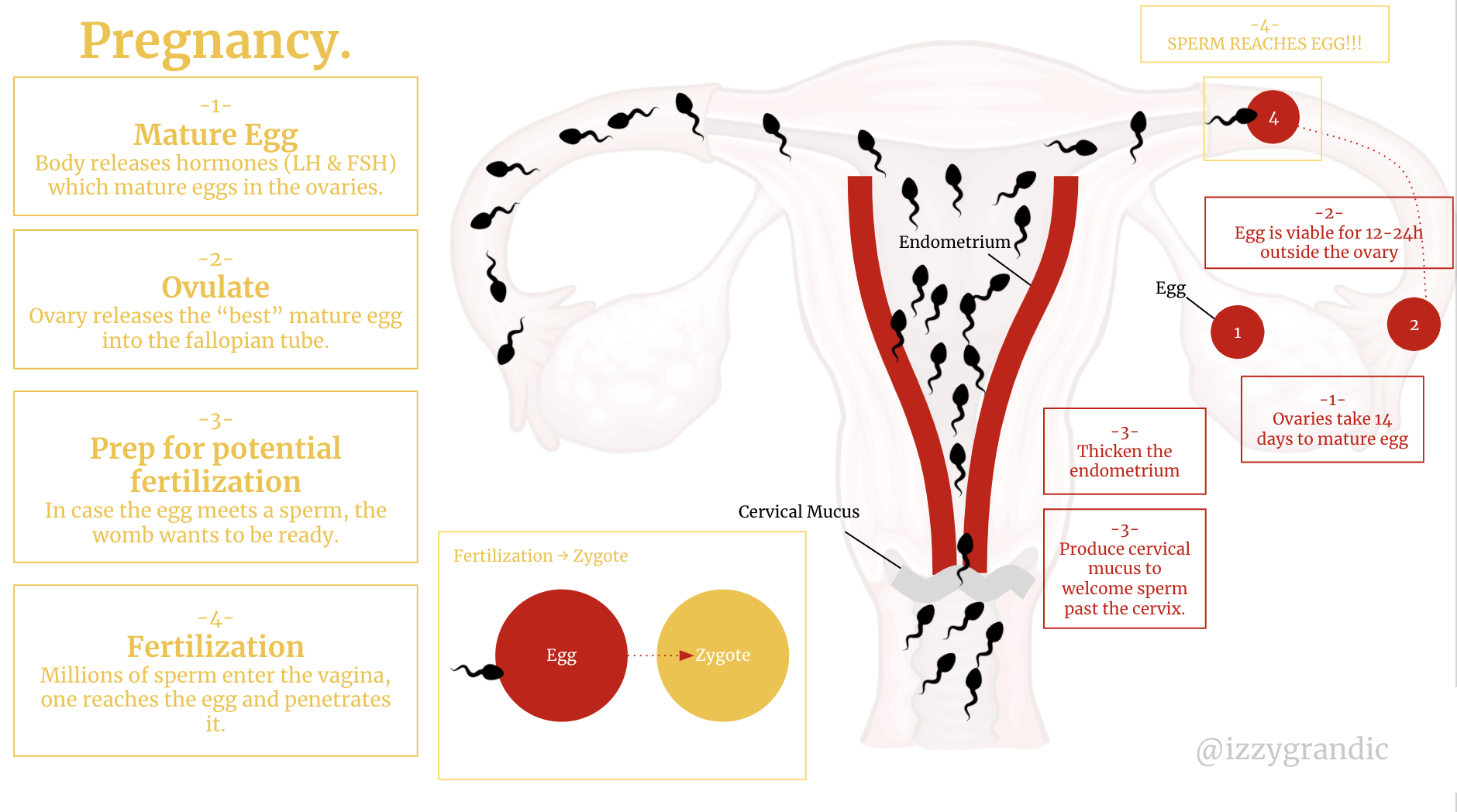 The first three steps are identical to menstruation. The only difference is fertilization happens, so the endometrium isn?t shed.
The first three steps are identical to menstruation. The only difference is fertilization happens, so the endometrium isn?t shed.
- That zygote spends a few days travelling down the fallopian tube, eventually implanting into the uterus.
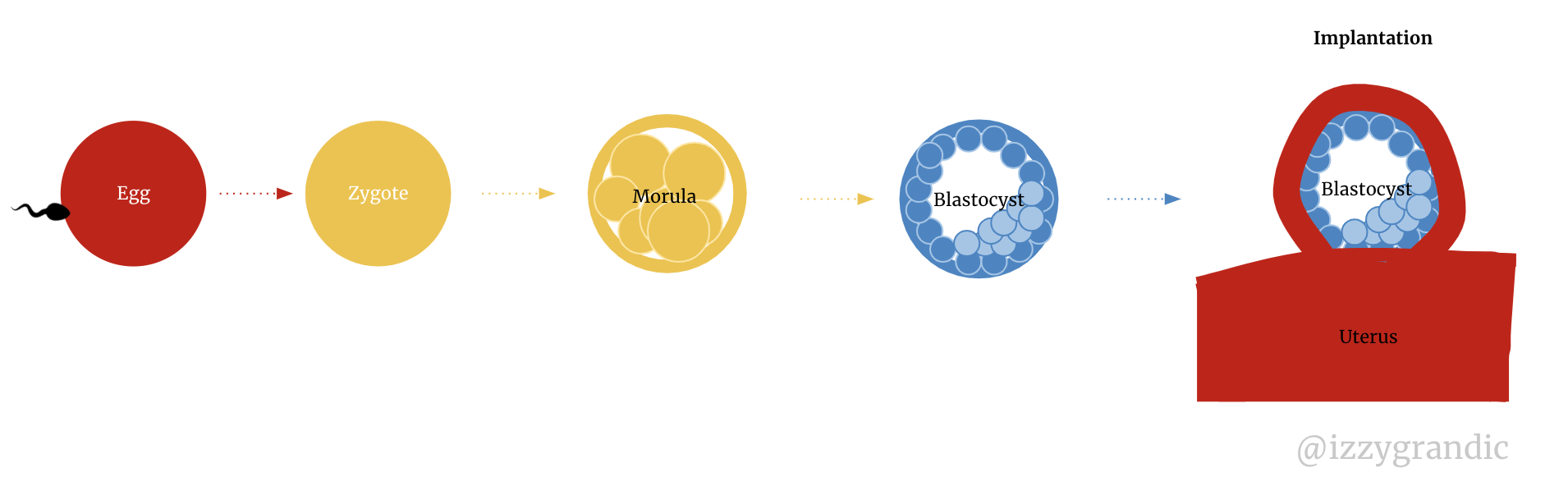 Zygote starts dividing (becomes morula). Then, as it continues to divide it becomes a blastocyst.
Zygote starts dividing (becomes morula). Then, as it continues to divide it becomes a blastocyst.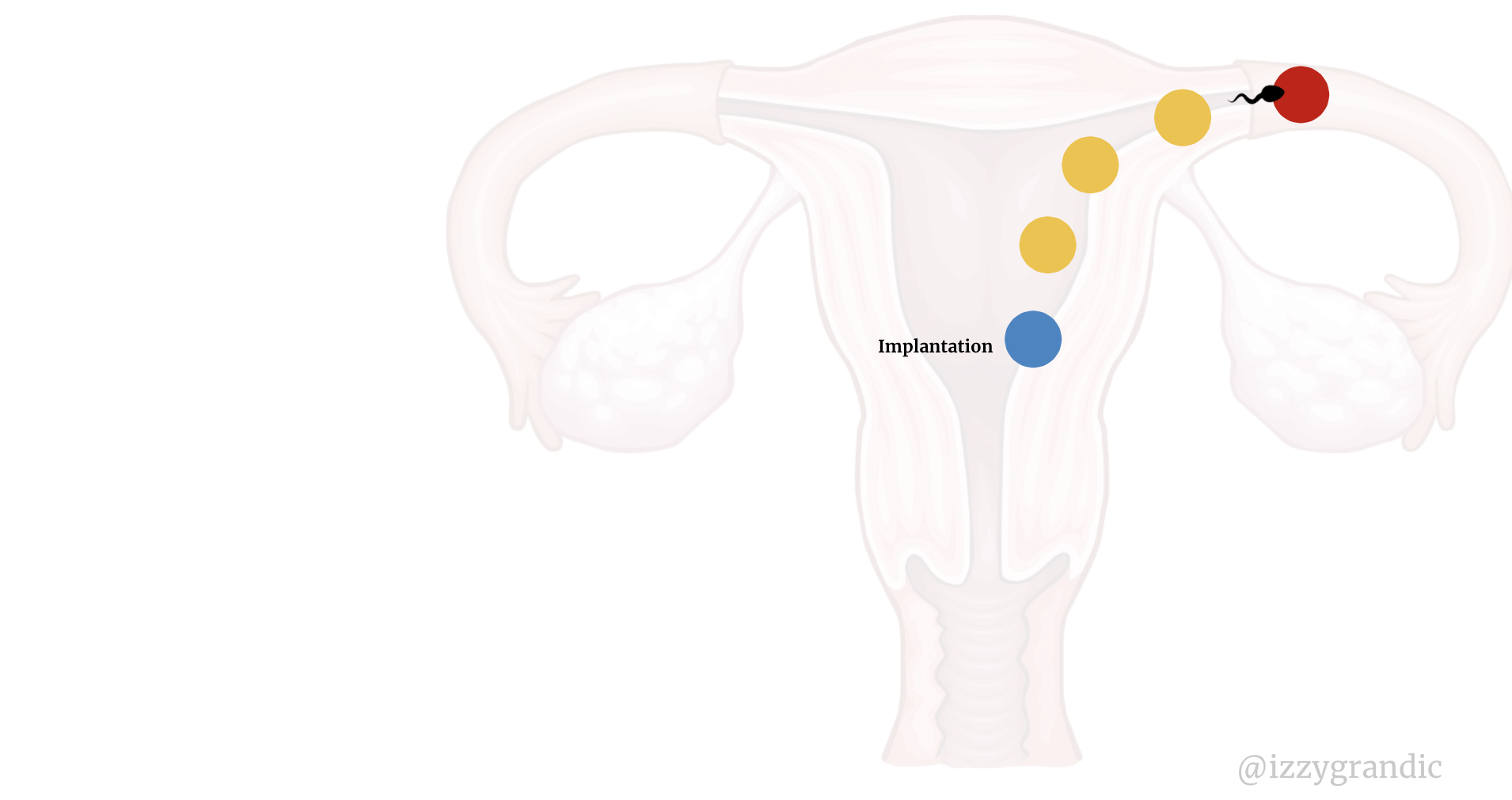 Implantation in action
Implantation in action
The quickest rundown:
Egg + Sperm = zygote ? gets implanted in uterus.
Sound familiar?
Eggo + Spermy Syrup = waffle snack ? gets implanted into your digestive system.
How come pregnancy doesn?t happen more often?
It?s a fair question. Given that 300M sperms enter the vagina, it seems highly likely that one will penetrate the egg, right?
But, there are still many obstacles in the body.
Sperm are going through a ?survival of the fittest? party. During ovulation (when the female body releases its egg), the female body creates a mucus. It?s thick, and the sperm need to swim through it; only the fittest survive.
When the sperm enter the tube, there?s a slight wind/force from the egg moving towards them. Eggs are 30x the size of sperms. For the sperms, it?s like running through massive wind storms. Another tough obstacle.
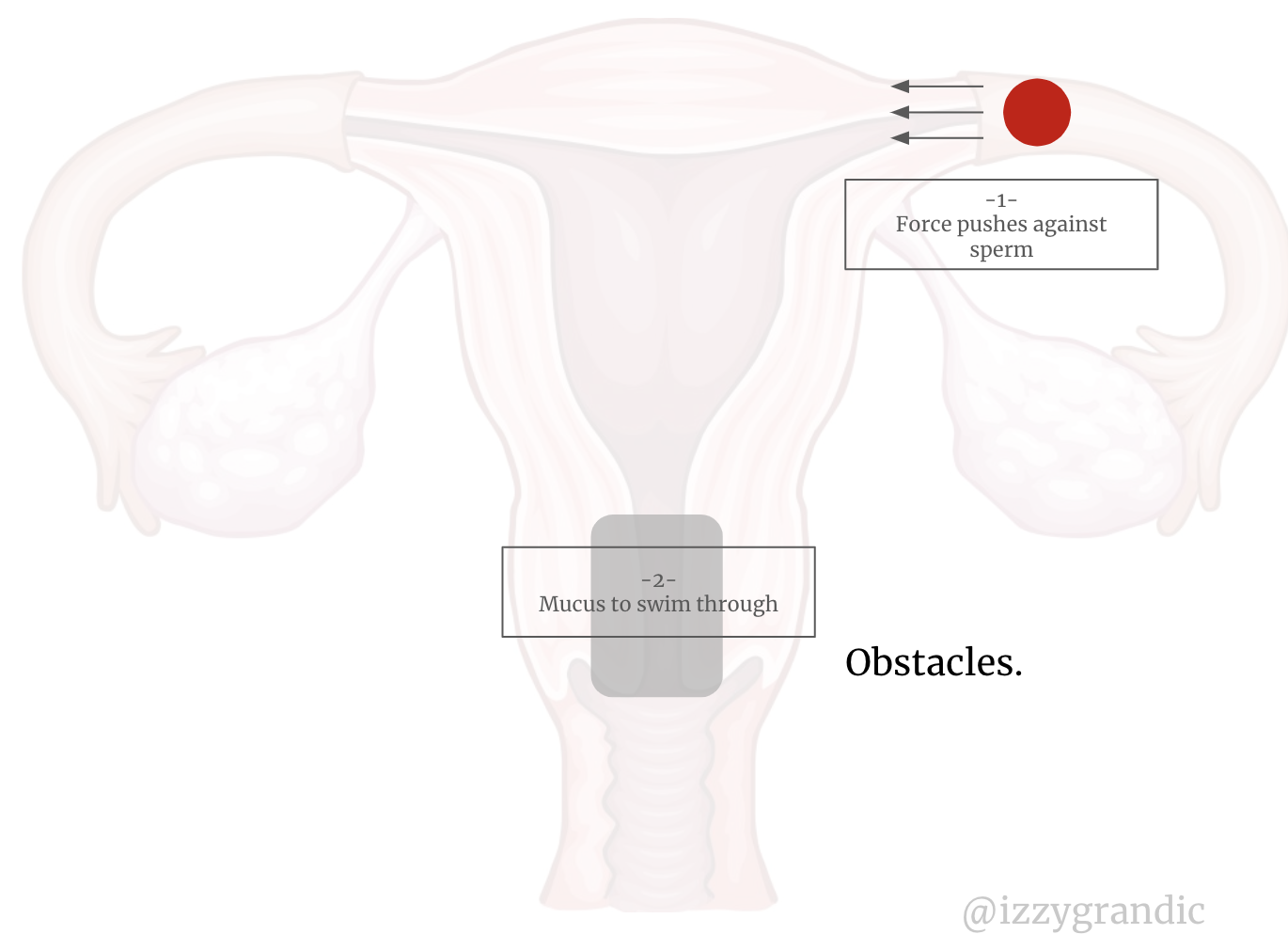
A woman is infertile most of the month. Her egg only has a 12?24h period when it can get fertilized.
If there?s no egg in the fallopian tube, no one is getting pregnant!
Most of the month, the egg stays inside the ovaries.
When the egg does leave the ovaries, it can only survive for 12?24 hours; pretty short window!
Now, sperm can survive a few days ?in there.? But because the window is so short, most die off before they reach the egg.
? It?s a timely process!!
There are different factors which can make it harder.
As we age, it?s harder to reproduce. Our bodies start to deteriorate. It?s harder for them to track hormones and other vital processes. Sometimes our diet, weight and genetics impact our reproducibility.
There?s a lot to discuss here; many different factors lead to infertility. This answer deserves its own section.
What causes infertility?
Infertility can be a confusing topic because it has so many interpretations.
Let?s make it clear: an infertile woman != sterile woman.
A sterilized woman is not able to have a baby.
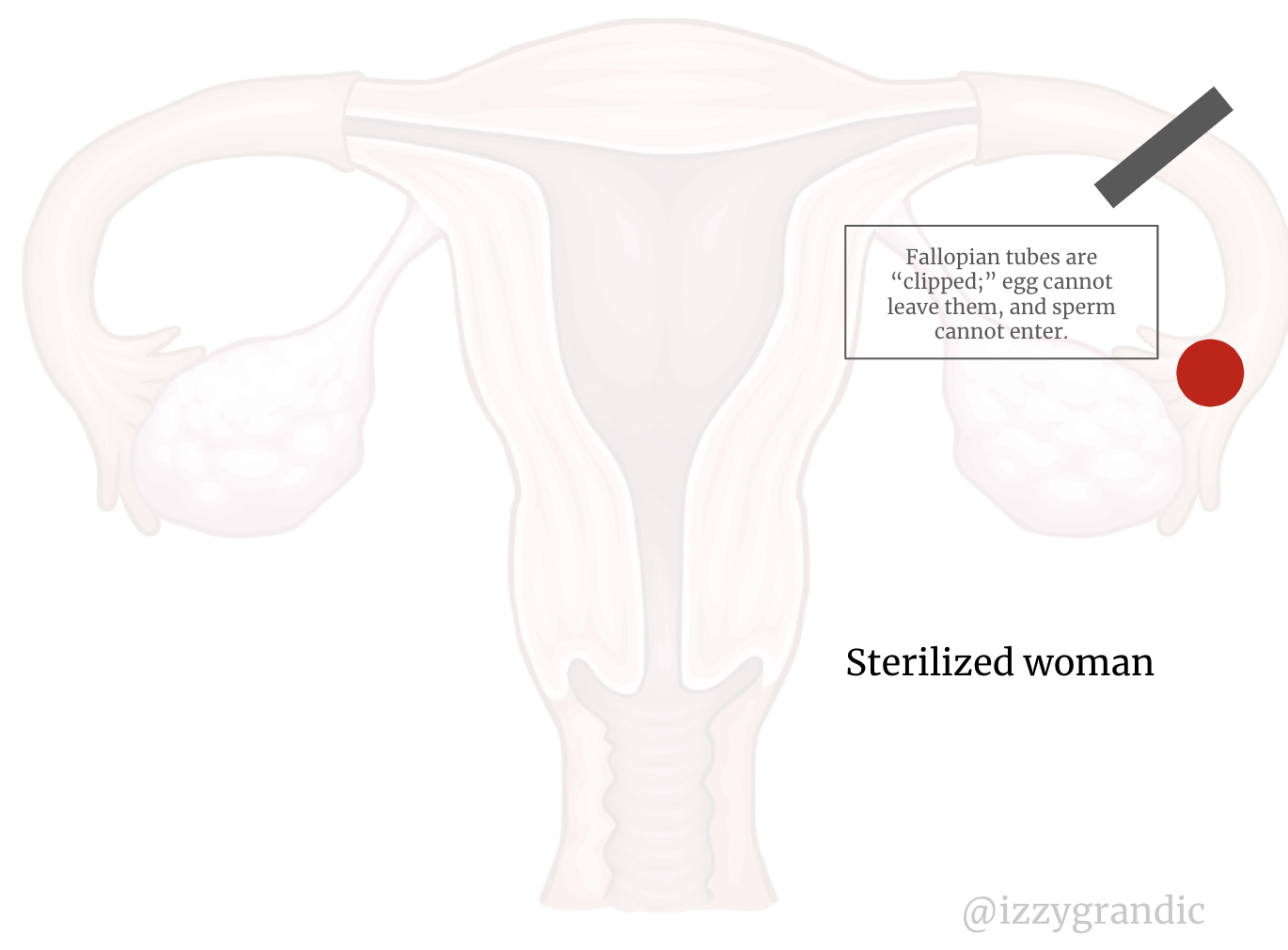
Someone that is infertile, has ?trouble? conceiving, and often needs some help. But, they are still able to have a baby. It?s just not a piece of w?a?f?f?l?e? cake.
For pregnancy to happen, we need 5 things:
- A mature egg in the fallopian tubes
- Balanced female hormones
- Sex near ovulation
- Functioning sperm
- Genetic compatibility between partners
Without these three things, it?s next-to-impossible to make a baby. Female infertility deals with the first two.
I?ll be writing about female infertility because this is a femtech article. Female infertility causes 1/3 of infertility problems. (Men cause 1/3, and the last third is ?unknown? problems that usually have to do with partner compatibility).
Issues with Female Fertility
Here?s the breakdown of what problems correlate to female infertility:
Ovulatory disorders = 35%
Tubal obstruction = 35%
Endometriosis = 20%
Idiopathic (unknown) = 10%
We know what causes 90% of infertility. What do each of these mean and how do they prohibit the syrup-waffle reunion?
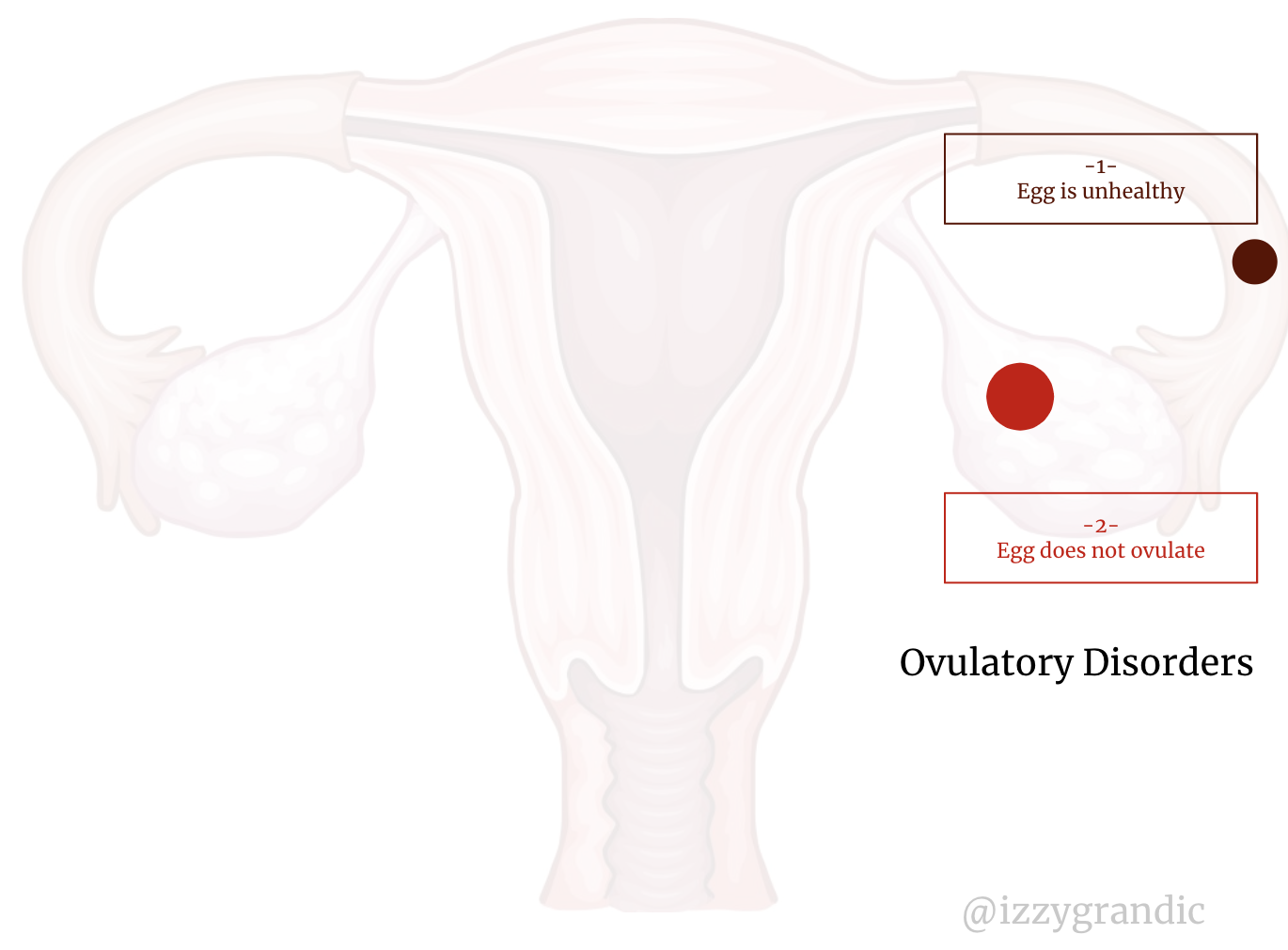
Infertility Cause #1: Ovulatory Disorders
These impact the egg (aka ovum). Common problems that arise:
- Egg doesn?t reach its age of maturity (it?s not ?healthy)
- Egg doesn?t ovulate (doesn?t leave the ovaries)
There are three classifications of ovulatory disorders.
- Hypothalamic Pituitary failure (producing little to no sex hormones)
- Hypothalamic pituitary ovarian dysfunction (disrupting hormone ? ovary communication)
- Ovarian failure
What causes ovulatory disorders?
Hormonal Imbalance
It?s difficult to keep your hormones balanced 100% of the time. Everything you do impacts your hormones in some way.
I like to think about hormonal balance/imbalance as a relationship between 2 people. It could be siblings, your parents, your friends, etc.
All relationships, at some point, have disagreements. No two people are the same, so they?re bound to not agree on some things. This, can lead to arguments. A few arguments can be managable. But, over time, too many arguments can ruin your relationship.
Lots of arguments = worse relationship. (Of course, there?s a ton of exceptions here, but bear with me for the sake of analogy).
There are things you can do to make up for the arguments. Like, take your friend out to dinner, make a nice card or apologize. These can make up for the disputes.
Lots of arguments + apologies = stable relationship.
Hormones work like our artificial relationship equations work.
Arguing with our bodies which causes imbalance. Sometimes, we never apologize so it worsens our relationship.
Hormones control ovulation. If hormones are functioning irregularly, so will your ovulatory cycle.
When your relationship with someone is going downhill, you tend to have bad days. You?re angrier or more anxious than usual. The same thing happens to your hypothalamus ? the part of your brain that controls hormones.
How do we argue with hormones?
Large/Shocking changes
Imagine you?re in a super-duper important work meeting. You have your fancy shoes on, and you have a collection of nice-looking charts. You?re ready to roll!
Yet, in the middle of the meeting, you get a message. It feels like your whole body is in shock; your mind is blank. One of your closest friends died.
No type of fancy shoes will stop you from feeling pain. You?ll be more distracted during your meeting. You might bomb it, actually.
But that?s what massive change does. It shifts your attention.
Your hormones are YOU in that meeting. The meeting is about preparing for ovulation. They need to be un-distracted to do the meeting well.
The diagram below represents your hormone?s goals. In the meeting, they want to talk about a strategy to achieve these goals.
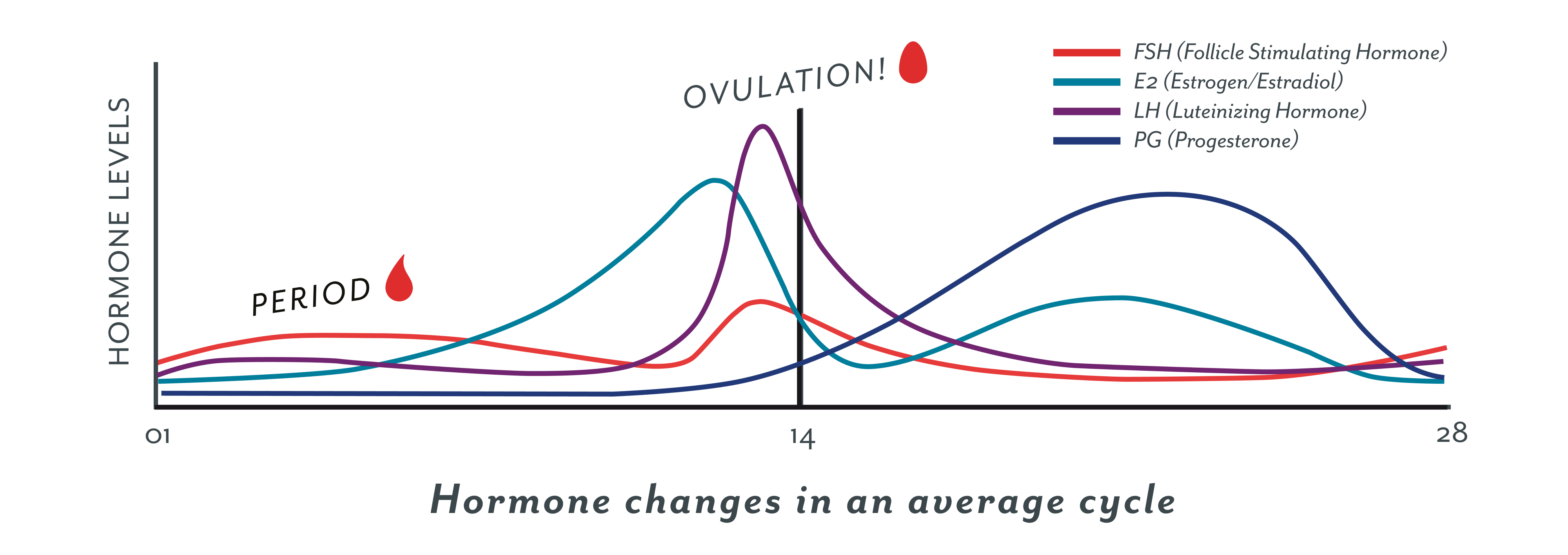 Women need this pattern of hormones to ovulate.
Women need this pattern of hormones to ovulate.
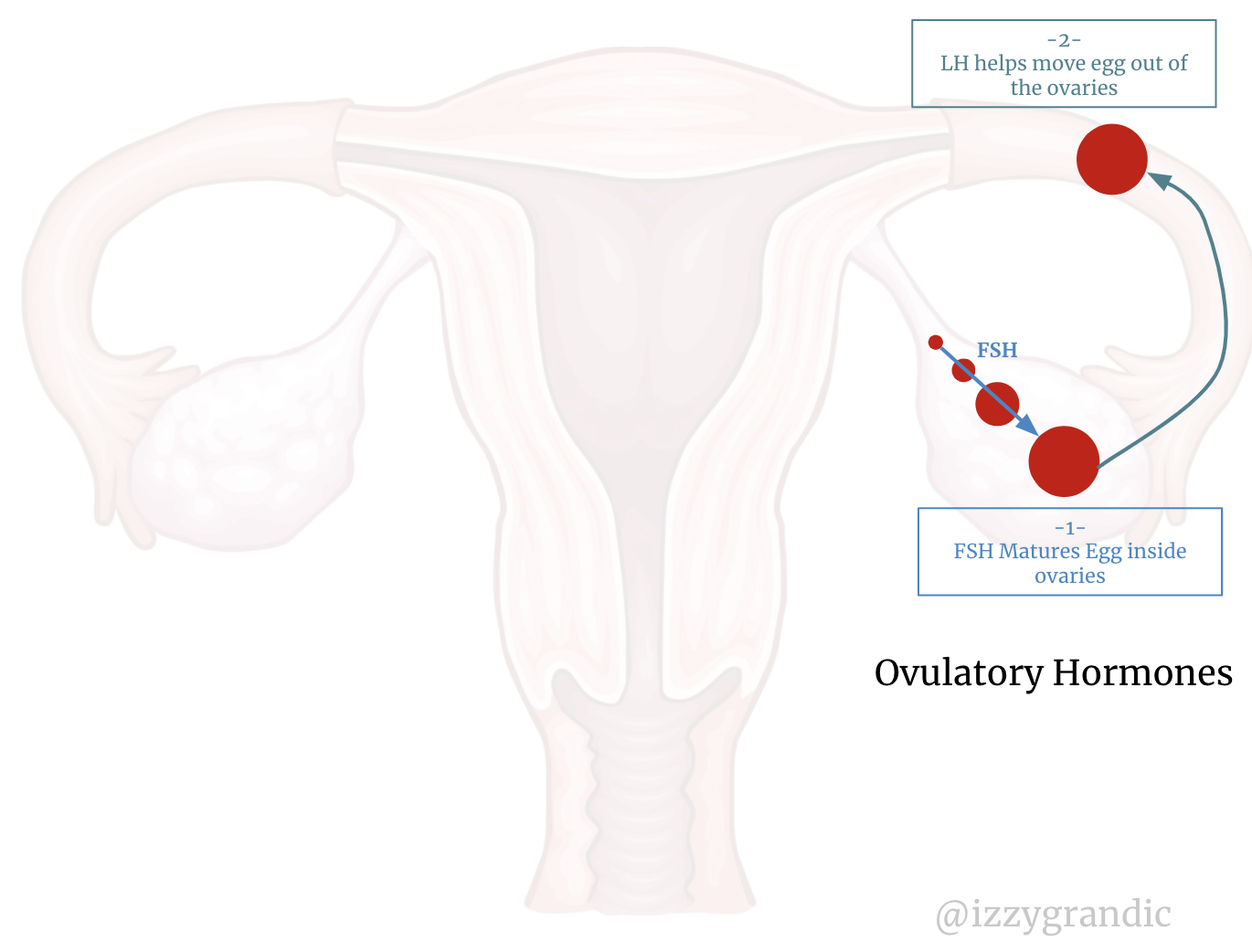
There are two important pre-ovulatory hormones: Folicle stimulating hormone (FSH) and luteinizing hormone(LH).
FSH matures your eggs and LH releases your eggs into the fallopian tubes. Normally your body regulates these. Both of these are regulated by the pituitary gland (in the brain).
But, if the body has extreme stress, the pituitary gland will pay less attention to FSH/LH levels. Since its attention is more focused on the area of stress.
Large stress factors include:
- Emotional stress.
- Weight gain/loss
- Physical stress
Sometimes, it?s not about a sudden stress factor. Often it?s several small stresses that build up. Some examples:
- Eating many transfats
- Caffeine
- Chemical exposure
From an evolutionary perspective, when ?times are tough,? your body knows it can?t handle reproducing.
For example, when one eats less, their body thinks they?re running out of food.
So, it turns on its ?longevity genes.? These are genes that promote living longer and decrease fertility. When you don?t have enough resources for yourself, your body knows it can?t house a child.
When you?re going through severe stress, your body has a similar opinion. Because your body senses so many toxins and dangers, it de-prioritizes reproduction to focus on survival.
If our hormones aren?t functioning, we may end up with hypogonadotropic hypogonadism. It?s a sophisticated way of saying ?our pituitary gland is producing little to no sex hormones.? This causes 10% of ovulatory disorders (3.5% of all infertility).
No hormones, no reproduction.
Polycystic ovary syndrome (PCOS)
PCOS is when a female has too many male hormones, which causes her ovaries to abnormally function.
Inside a woman?s ovaries, she?ll have many cysts. That?s why it?s called ?poly? (many) ?cystic? (cysts).
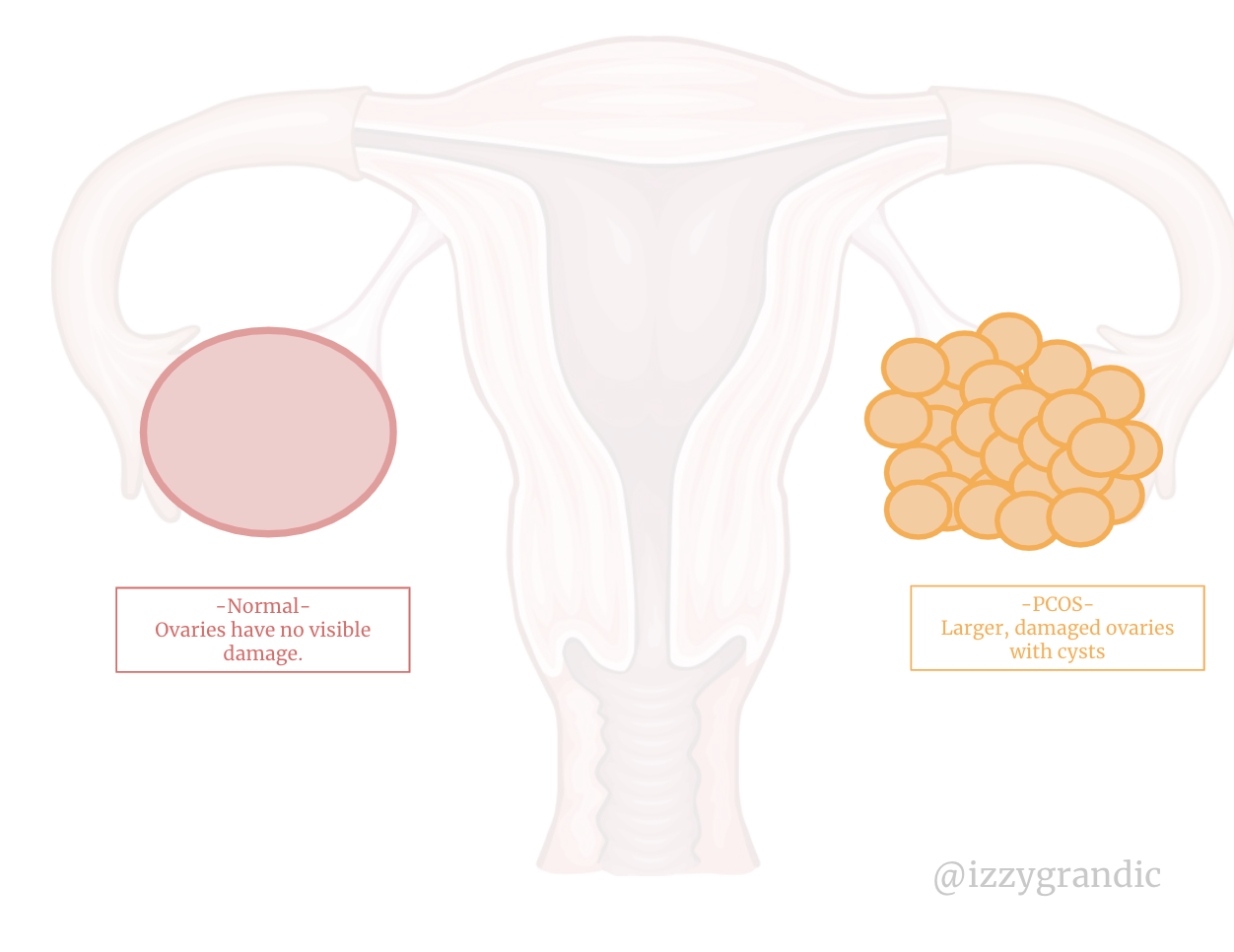
It causes two main problems:
- Stops eggs from maturing (properly) in the ovaries.
- Stops eggs from exiting the ovaries. This usually results in irregular/missed periods.
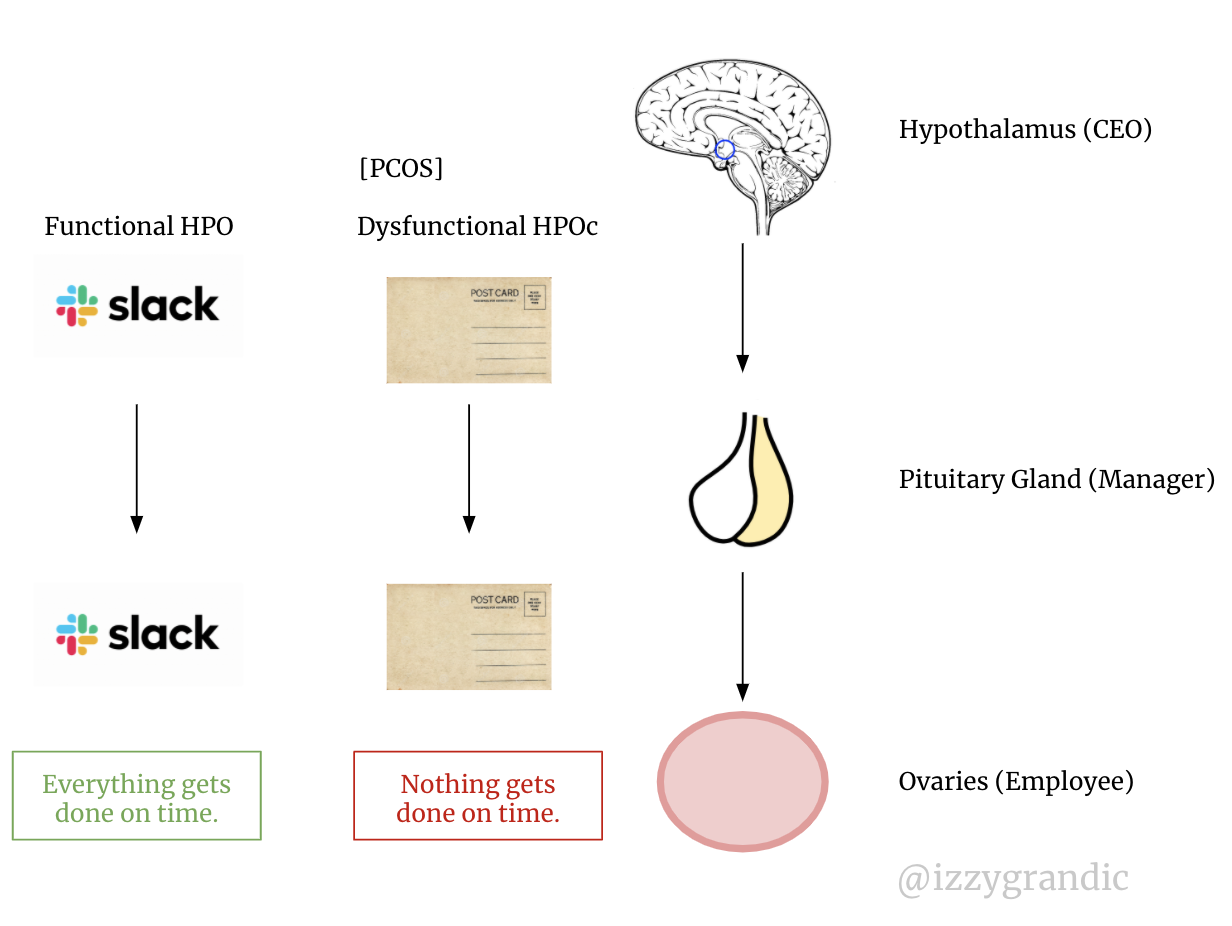
PCOS causes a dysfunction of the hypothalamic-pituitary-ovarian (HPO) axis. The dysfunction of HPO makes up 85% of ovulatory disorders (29.75% of all infertility).
What does it mean to disrupt the HPO axis?
Think of the hypothalamus as the CEO; pituitary as the manager; and the ovaries as an employee.
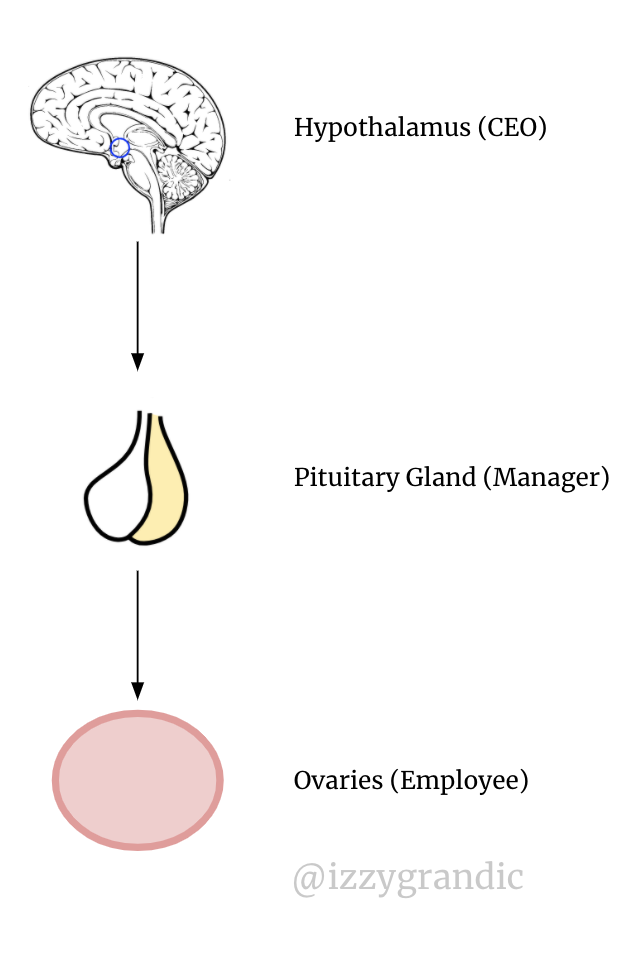 HPO axis
HPO axis
Because I?m writing this during the COVID-19 pandemic, each of them are WFH (working from home). A properly functioning HPO axis uses slack, email or another convenient messaging platform.
A dysfunctioning HPO axis uses postcards (in 2020) to deliver messages. Yikes. You?d get letters and updates days later; it?s an inconvenient system. There?s a reason Slack is a multi-billion dollar company.
 I think I just changed the game for Slack?s endocrinology targeted ad strategy.
I think I just changed the game for Slack?s endocrinology targeted ad strategy.
Why do some women get PCOS? Well, we?re not sure, but the leading hypothesis is that these women have excess male hormones.
Other ovarian-disorder contributors
Toxins. Cigarette smoking, pesticides, viruses, etc. Smokers are 60% more likely to be infertile
Genetics. Disorders like mosaic Turner syndrome affect the function of the ovaries.
Immune system failure. Your immune system thinks your ovaries are dangerous. It triggers an auto-immune response to ?kill? the tissue. We don?t know why this happens.
Primary ovarian insufficiency. This is when a woman?s ovaries fail. 90% of the time we don?t know the cause.
Age. As a woman gets older, the # of eggs she has declines. Having fewer eggs can cause the ovaries to behave oddly. A woman?s chances of conceiving decrease 3?5% per year after age 30.
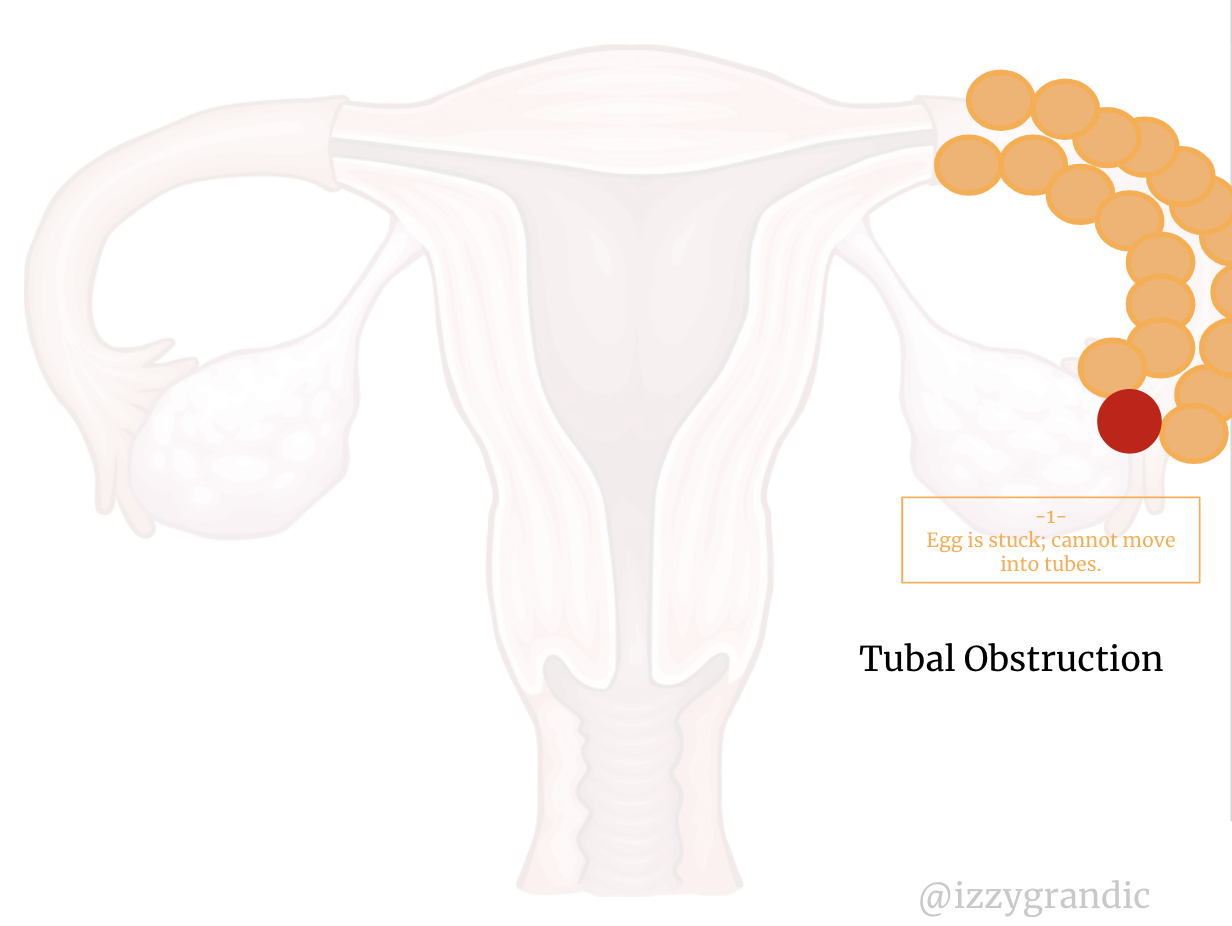
Infertility Cause #2: Tubal Obstruction
If we block the toaster, the waffle can?t go inside. If it can?t go inside, there?s nothing to ?toast.?
If there?s a fallopian tube blockage, the egg is in a bit of a pickle. It?s unavailable to the sperm. 🙁
What causes this blockage?
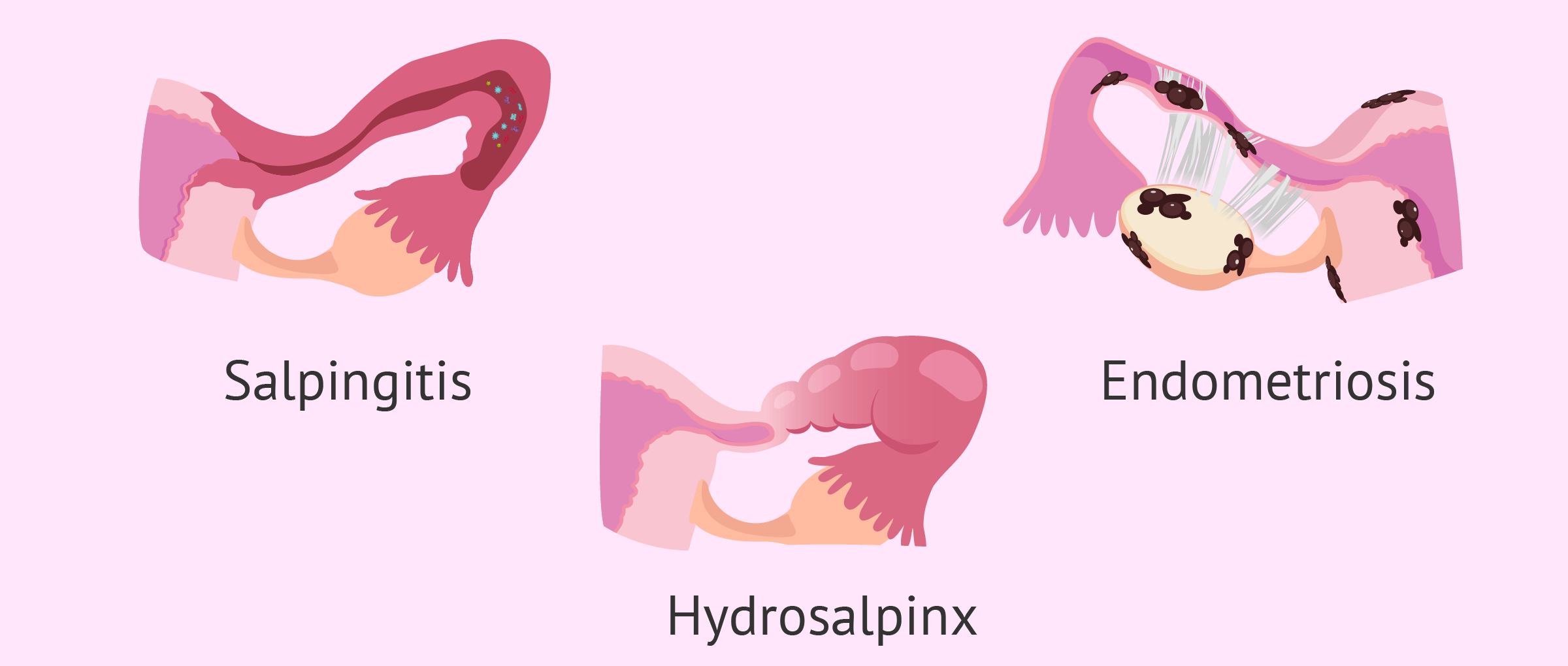 Some examples of blockage
Some examples of blockage
TLDR: any form of inflammation or tissues that build up in the tubes. Inflammation causes swelling, which decreases the opening of the tubes. Different diseases/conditions cause a pile-up of muck in there.
But, more specifically?
Pelvic Inflammatory Disease (PID) / Sexually Transmitted Infections (STIs)
PID is like an allergic reaction in your pelvic region. When foreign bacteria come in (say, through STIs) your body starts to freak out.
Most commonly, gonorrhea or chlamydia can block fallopian tubes.
It causes swelling and a burning sensation whenever you sit down.
Even if you don?t presently have PID, a history of PID can put you in danger of tube blockage/infertility.
Scar tissue
If you?ve had surgery near the reproductive area, you?re at risk for tubal obstruction. Scar tissue, infections, etc., all impact how well your system functions.
Any disruption, like the invasion of sharp metal objects, is risky for fertility.
Hydrosalpinx
This is a water build-up in the fallopian tubes. It?s often caused by surgery or PID.
One last potential cause of tubal obstruction is endometriosis. But, it?s such a colossal factor of infertility (20%), it?s getting its own section.
Infertility cause #3: Endometriosis
Endometriosis is like a dog with short-term memory loss. It has ?cute? intentions, but very poor execution. This dog?s actions are very confusing.
 Everyone meet endometriosis, the lost and confused dog.
Everyone meet endometriosis, the lost and confused dog.
It runs into walls. Pees every 9.5 seconds. And, goes to catch a frisbee, but forgets what it?s doing as it runs towards the frisbee, which falls on its head.
?Endometri? refers to the endometrium. It?s the outer layer of the uterus that sheds monthly (aka the period). ?Osis? means ?condition.?
Sometimes the endometrium (in the case of endometriosis) grows in novel places. It spreads to the other parts of the reproductive system, like the outside of the ovaries.
Endometriosis is when the body grows the endometrium in places beyond the uterus. Why is this bad? During ?that time of the month,? hormones trigger all endometrial tissue to shed.
That means that the endometrium beyond the uterus will shed, but the blood will have nowhere to go. It?s internal bleeding ? and as you can imagine, very painful.
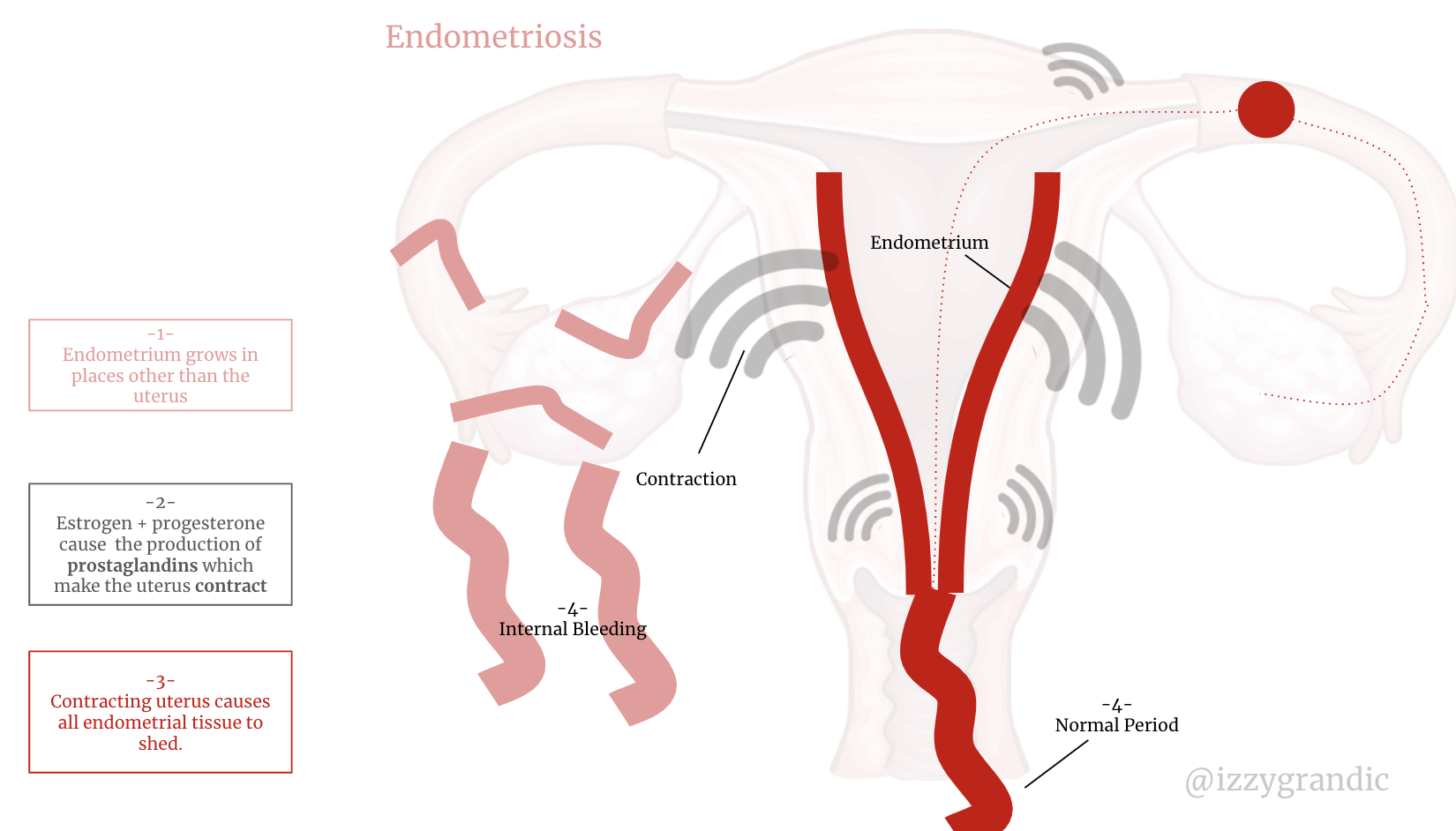
So, not only are women externally bleeding, several are internally bleeding too.
The endometrium forgets where it?s supposed to be.
How does this impact fertility?
TLDR: Endometriosis can block the fallopian tubes and inhibit ovulation.
Endometriosis has similar impacts to fertility as ovarian disorders and tubal obstruction. It can actually contribute to either of those.
There?s tons to learn about endometriosis. Here?s a good article to get started.
What solutions to infertility exist today?
There are so many ways we can negatively impact [female] fertility. But, we have some solutions.
I?ll be going over 3 medical solutions. There are other ?alternatives? like acupuncture and herbal medicines that we can use ? but these are more like ?supplements? rather than solutions.
Artificial Insemination
Insemination means the introduction of sperm into a female?s body. Artificial insemination means introducing sperm into a woman without sexual intercourse.
If you?re familiar with the show Jane the Virgin, you know exactly what I?m talking about 😉

There?s different ways we can artificially inseminate someone.
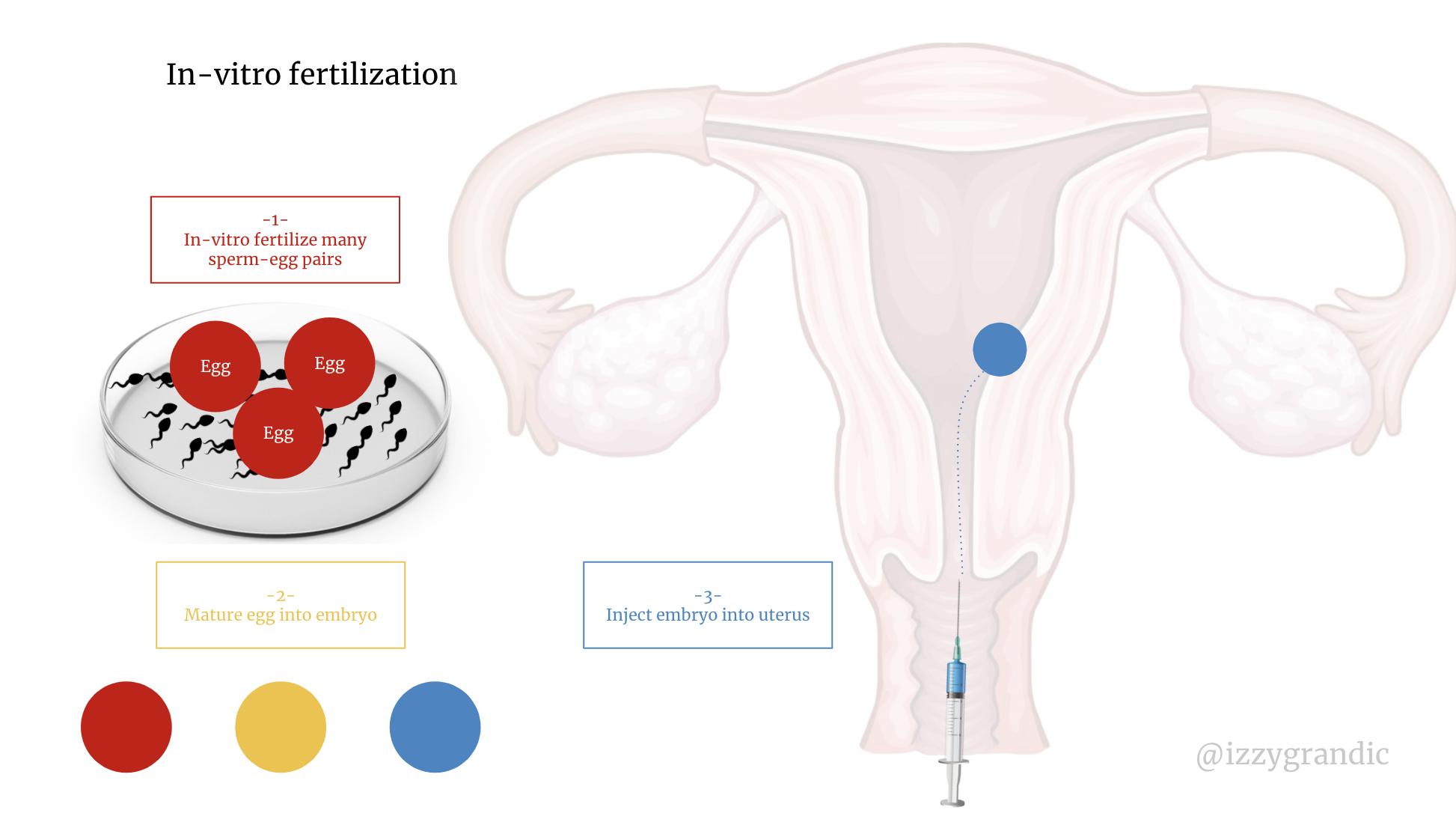
IVF (In-vitro Fertilization): Test tube Babies
The process:
- Combine egg + sperm in a dish to create embryos
- Place embryos in the uterus
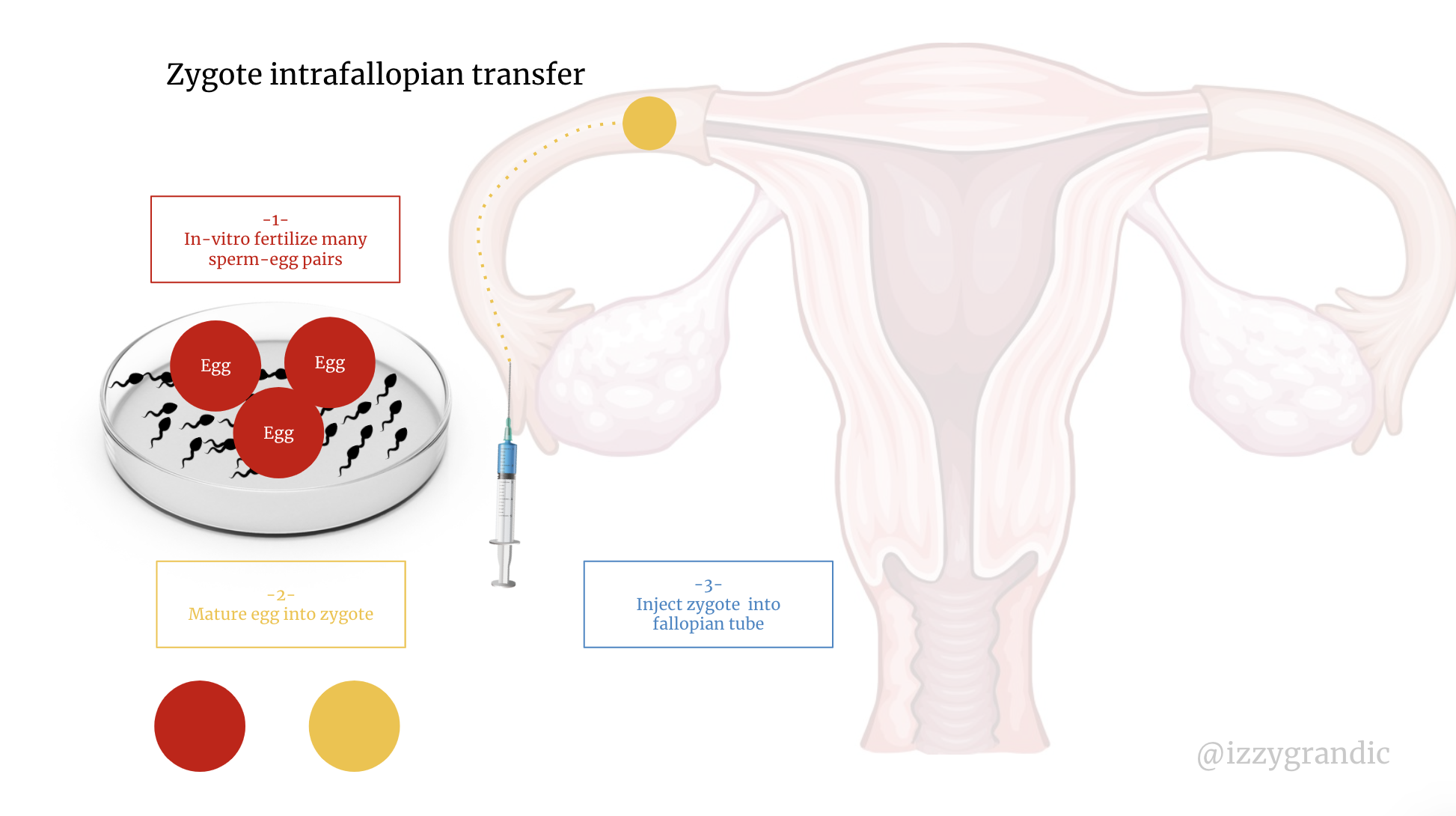
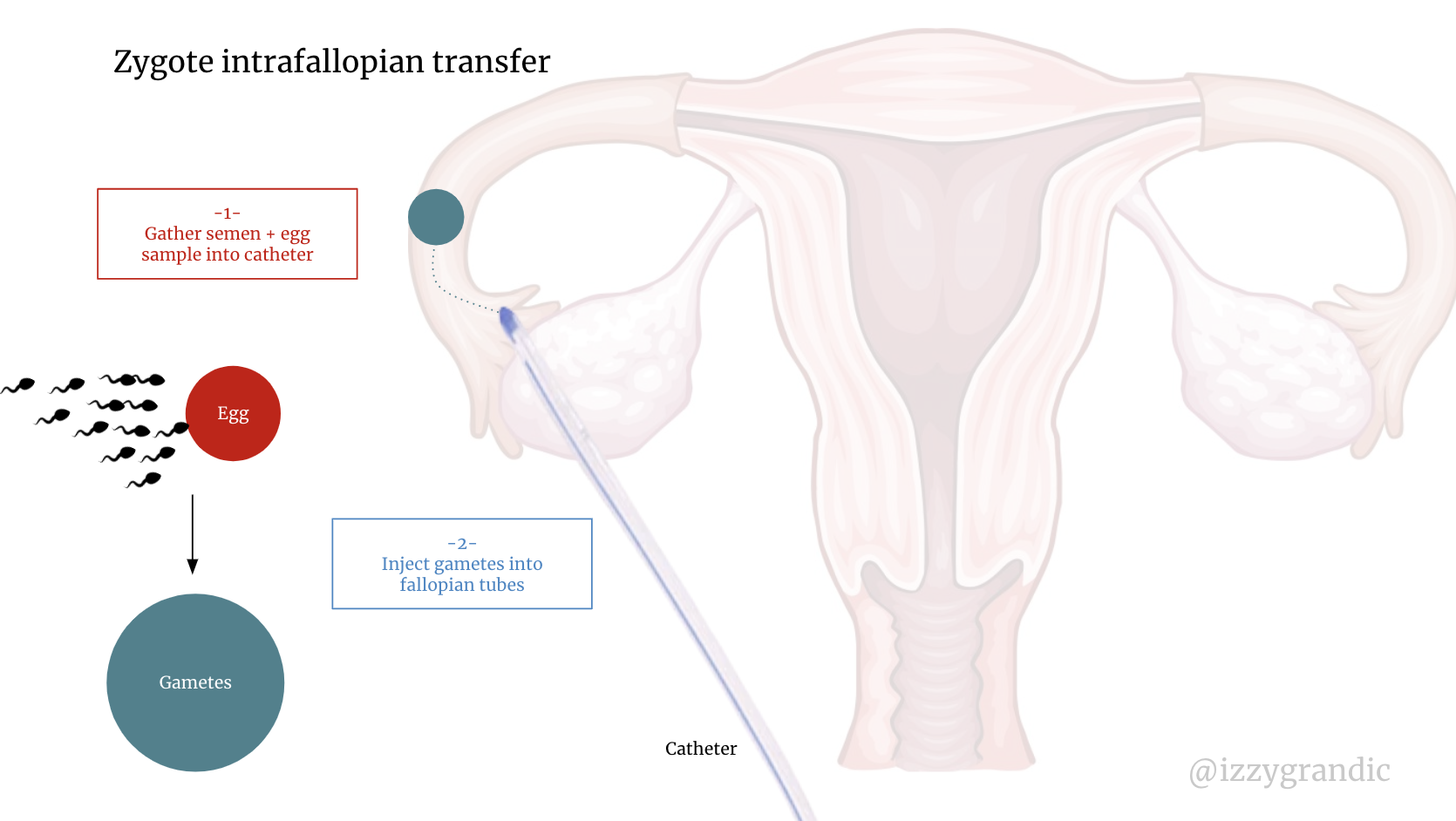
Zygote intrafallopian transfer (ZIFT):
The process:
- Combine egg + sperm in dish to create a zygote
- Place embryos in fallopian tubes
Gamete intrafallopian transfer (GIFT):
The process:
- Place gametes (sperm and eggs) into fallopian tubes
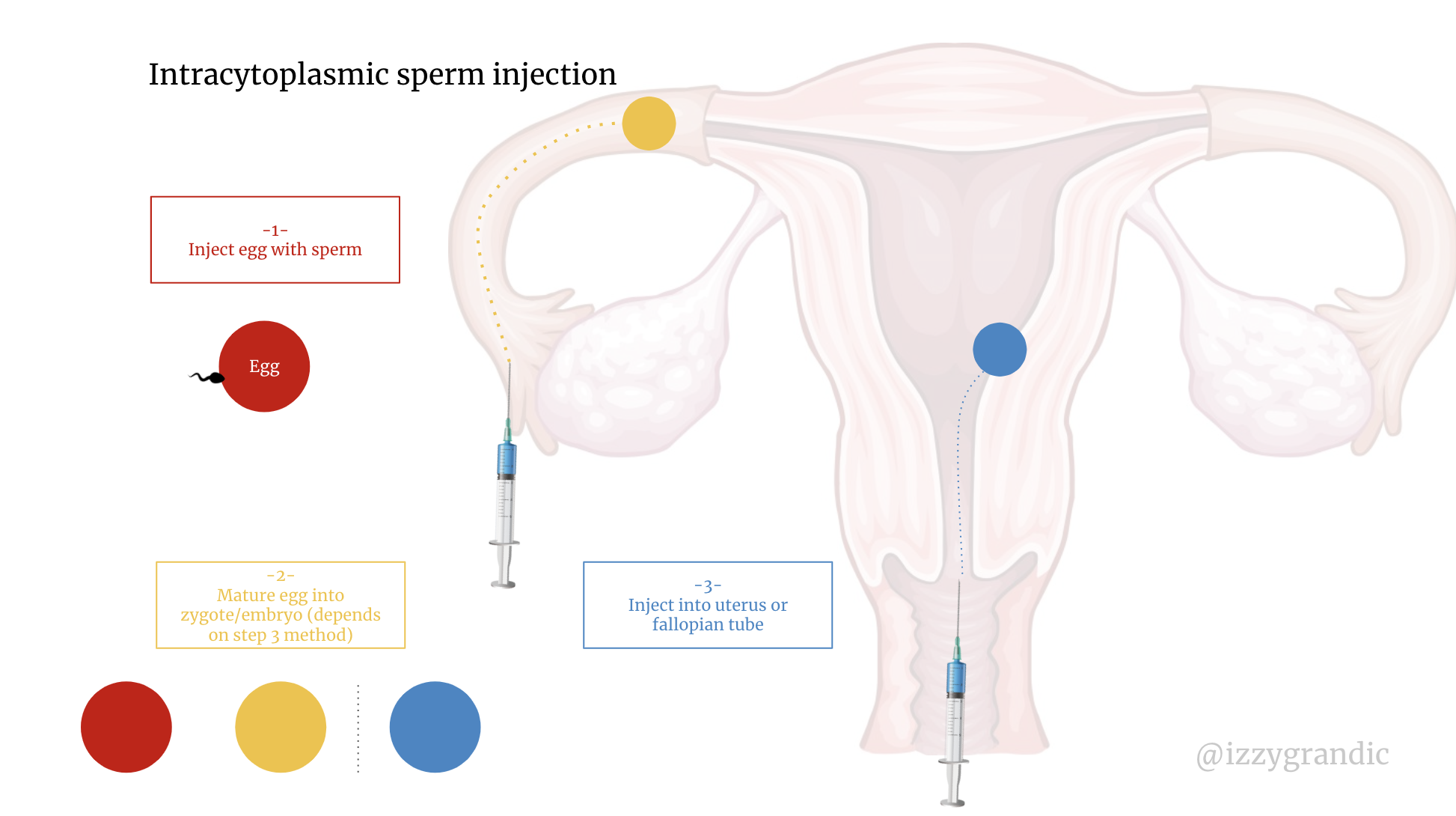
Intracytoplasmic sperm injection (ICSI):
The process:
- Inject egg with a single sperm
- Placed in fallopian tube or uterus
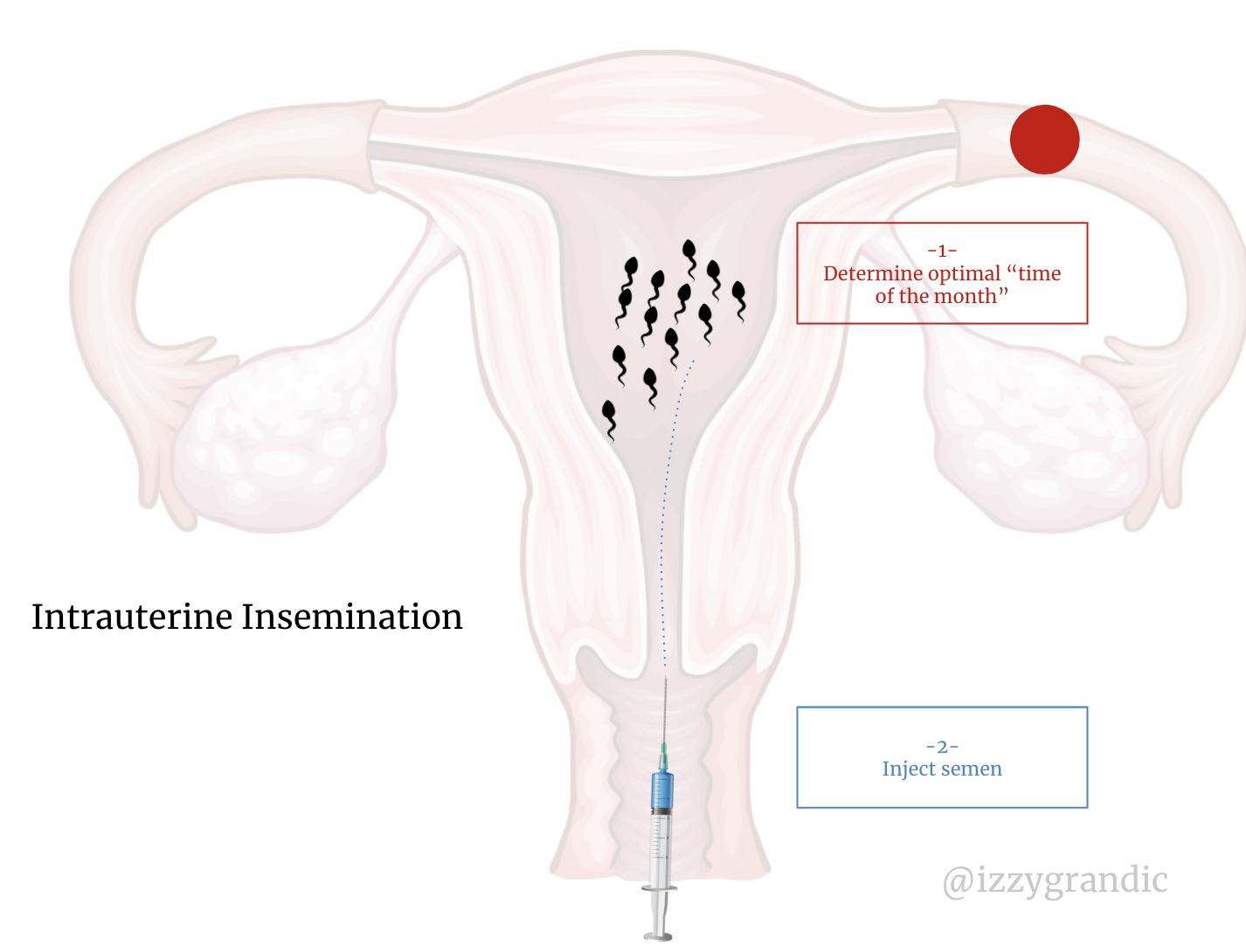
IUI: Intrauterine Insemination
The process
- Inject several sperm into the vagina at the most optimal time of the month.
There are different variations of artificial insemination. But, all boil down to taking luck out of the equation and ?cutting the line.?
Instead of spraying and praying for sperm to go in, some methods put the sperm in the embryo. This saves time.
Instead of hoping for the embryo to make it into the uterus, some methods place it right in there.
Drug Therapy
These are drugs that trigger changes in hormones.
Anti-estrogen (clomiphene citrate)
- Increases GnRH, FSH & LH
- Why are these important? GnRH stimulates the production of FSH and LH. FSH helps the ovaries mature its eggs; LH helps the eggs ovulate; both crucial to conception.
- Often, infertility occurs when we lack one (or more) of these 3 hormones.
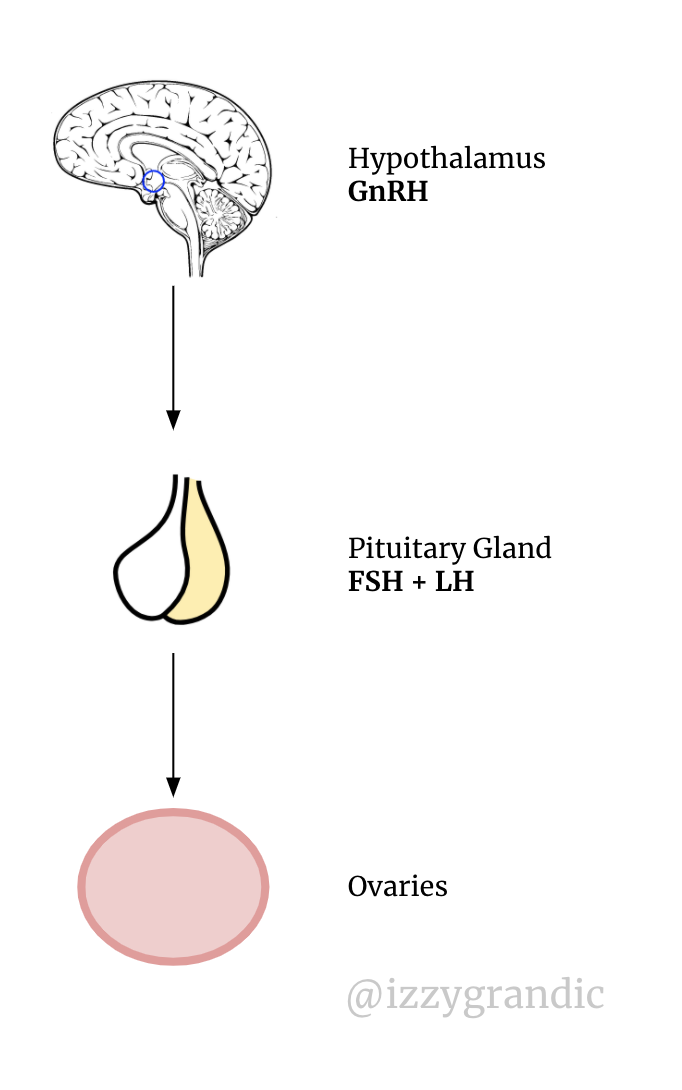 GnRH monitors the release of FSH/LH.
GnRH monitors the release of FSH/LH.
Metformin: supplementary drug to clomiphene; makes its effects more effective than clomiphene alone.
- Reduces androgen (male hormone) levels
- Why lower androgens? Androgens are male sex hormones. When females want to produce, they need more female sex hormones.
Bromocriptine/Cabergoline
- This drug lowers prolactin levels.
- Why lower prolactin? Prolactin is the hormone that regulates milk production. After a mother gives birth, her prolactin levels are high to help her produce milk for breastfeeding; while stopping ovulation. High prolactin levels = little to no ovulation = difficulty getting pregnant.
Hormones
These are direct injections of hormones
hMG: combines LH + FSH to stimulate the ovaries
FSH analog: stimulates FSH
Gn-RH analog: stimulates Gn-RH (rarely prescribed)
HCG analog: Triggers ovaries to release its eggs
TLDR: we want to increase FSH/LH (or Gn-RH, which does this anyway). Why? Because these are the hormones involved with creating and releasing eggs.
These hormones stimulate the ovaries, which help them do their job.
Adding extra hormonal therapy is like giving a hearing aid to an elderly person. It amplifies ?noise? so they can hear. Hormonal therapy amiplies ?stimulus? so the ovaries can mature eggs and ovulate.
How can femtech advance conception?
Improving timing accuracy. The truth about pregnancy is it takes a lot of tries.
If a woman is under the age of 35, she?s not ?infertile? until she?s tried to get pregnant for 1 year. Meaning to be considered infertile, she has to have frequent sex for 1 year with no pregnancy luck.
Couples need to try often, ?to get the timing right.?
The more a woman can understand when she?s ovulating, the more likely she can ?time? trying to get pregnant.
Improving reproductive organ function. If there are challenges in the reproductive system, getting pregnant becomes harder. For example, 70% of women with PCOS don?t know they have it.
Women should have more direct knowledge of their reproductive health anyway. We need more at-home testing and proactive ways for women to watch their reproductive system.
Identify any problems sooner. We don?t understand most of these diseases. 10% of female infertility causes are unknown. 33% of all infertility causes are unknown.
In the future, we?ll have more data collection and more algorithms running on that data. We?ll find issues sooner. To live in this world, we need to focus on two things:
- Collecting Data
- Building Algorithms/Models for that data
Managing hormones. Ah. Our good friends that we don?t know how to use. From my understanding of hormones and women?s health, we?re far off from understanding its full function.
Hormones are one of the most important players in conception (and all things reproduction). ? WE NEED TO KNOW MORE.
Making solutions more affordable. Only 5% of couples with infertility issues use IVF. It costs tens of thousands of dollars, so that low figure isn?t surprising. Right now, fertility options are available to a few people, but we should aim to make them available to many.
Pregnancy.
And, after $33 000 invested into IVF rounds, you?re pregnant! Now what?
Now, you?re growing a human inside of you ?. No big deal.
OK, it?s a big deal and there?s a whole new set of hurdles with pregnancy.
Let?s start with what actually happens in your body once that sperm and egg meet.
- Fertilization: Sperm & Egg meet. They combine their genetic information to form a zygote (single-celled organism).
- Implantation: the zygote divides to form a blastocyst. The blastocyst travels from the fallopian tubes to the uterine wall.
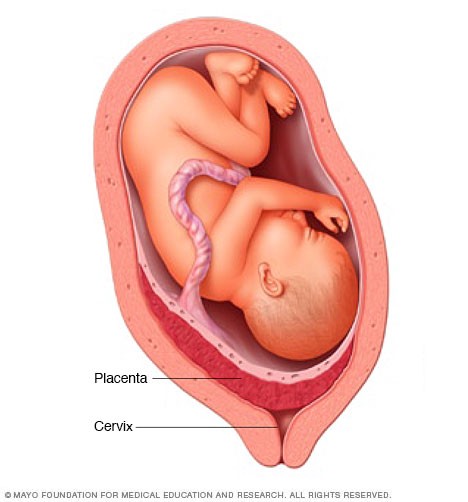
- Development: once the blastocyst implants into the uterus, it starts to develop into the placenta and uterus. The placenta is an organ that gives oxygen/nutrients to the developing baby. The blastocyst is an embryo once the amniotic sacs develop.
- Embryonic development: this is the phase where most organs form. The cell remains an embryo until ~11th week of pregnancy. It becomes a fetus.
- Fetal development: fetus develops until birth.
 ?
?
TLDR:
Zygote ? blastocyst ? placenta + embryo ? fetus ? newborn
I want to focus on the placenta for a moment. A woman?s body not only grows a child but an ORGAN too.
The placenta acts as a respiratory, digestive, hormonal and immune system for the baby.
Every pregnant woman deserves a big fat hug for growing a baby and an organ.
Pregnancy can be confusing, overwhelming and surprising. Here?s what I?ll go over in this section:
- Accidental pregnancies & abortions
- Miscarriages
- Maternal Death
- Maintaining health
Sometimes it?s accidental.
Actually, oftentimes it?s accidental. 50% of pregnancies in the US are unintended. Half of the unintended pregnancies used some form of contraceptive.
We?ve all heard the story about those silly teenagers in the hot tub, or the one time a woman had a one night stand. It happens.
Especially given that condoms are only ~80% effective (2 in 10 women will get pregnant). And, the pill is ~90% effective (1 in 10 women will get pregnant).
Women abort 43% of these unplanned pregnancies. Abortion is another form of contraception when all other forms fail.
The purpose of contraception is to give women control over their fertility. That?s what abortion does. Whether you?re pro-life or pro-choice; abortion is a contraceptive.
I?m not going to go too deep into the pro-life vs pro-choice debate. What I will say is making it illegal doesn?t make it go away.
Every year there are 56M abortions globally.
25M are classified as unsafe abortions (most of these are illegal). 68 000 of these abortions result in maternal death, 5M suffer long-term complications.
In El Salvador, abortion is illegal, yet 1 in 3 women still abort.
Each woman has their own reason for abortion; financial, timing or ?father issues.? 14,000 women in the US have abortions following rape or incest.
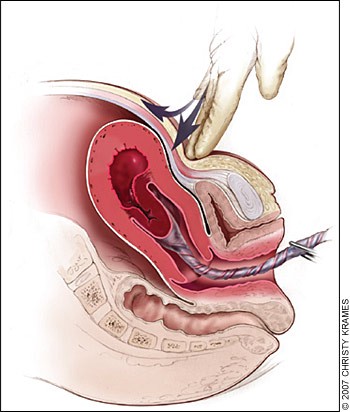
In countries where abortion is illegal, doctors may refuse to treat ectopic pregnancies. These are pregnancies where the fetus starts growing in the fallopian tubes rather than the uterus. They?re dangerous for both the mother and the baby.
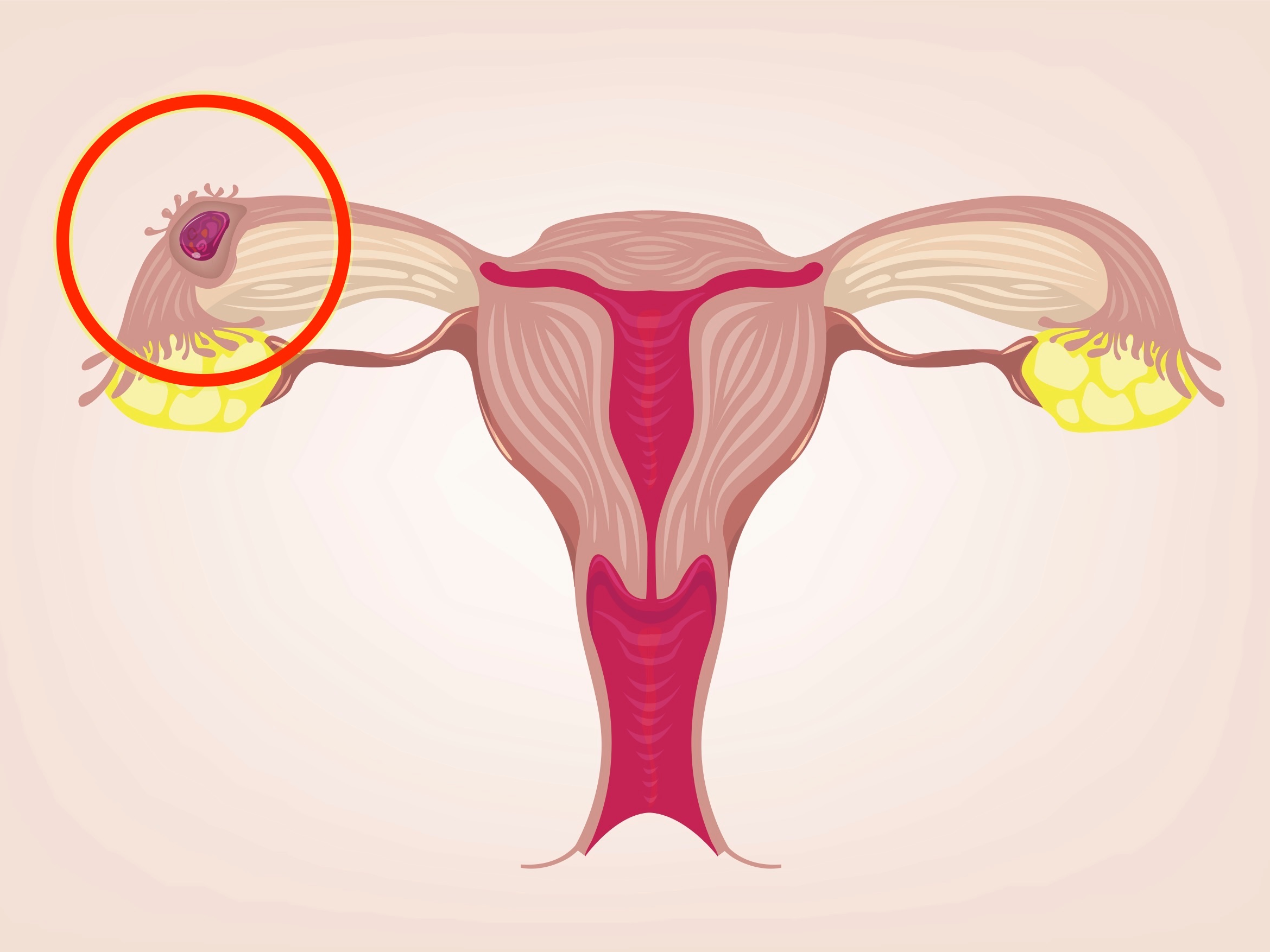 Ectopic pregnancy (top left corner)
Ectopic pregnancy (top left corner)
Instead of aborting early on, some believers think the woman should ?wait it out? until she miscarries. This is literally life-threatening.
Whether we like it or not, abortion is something millions of women will choose. The only difference is safety.
97% of dangerous abortions happen in the developing world. Coincidentally, that?s where abortions are most illegal.
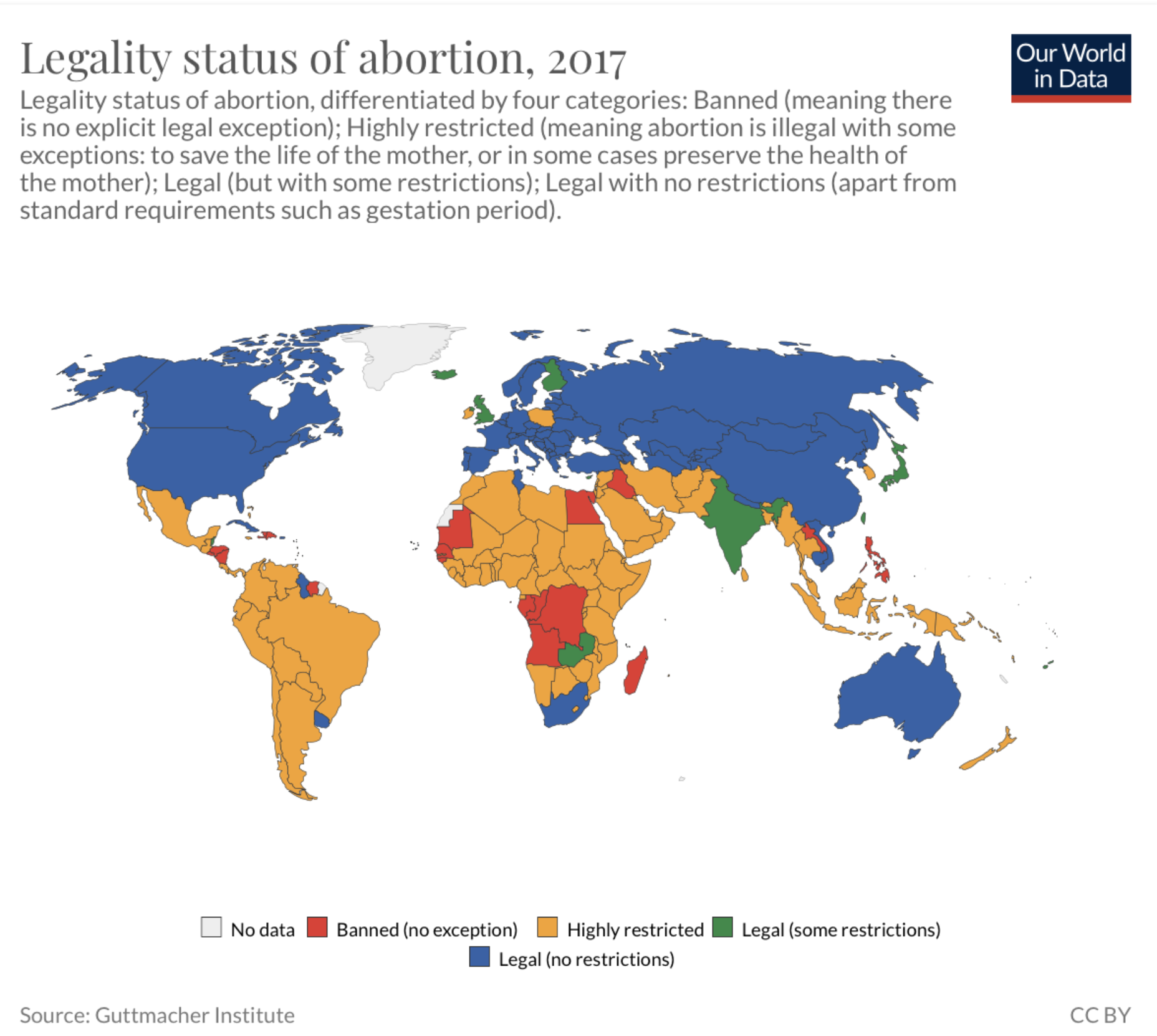
How can we reduce the # of unintended pregnancies per year? Easier, cheaper access to contraceptives. Without publicly funded contraceptive services, there would be 40% more abortions each year in the US.
If women who don?t want to get pregnant in the first place don?t, that would be the most ideal situation.
If every woman gave birth to the aborted pregnancies, we would almost double the maternal mortality rate. 259,120 more mothers would die/year.
13% of maternal death is because of abortion. Maternal death impacts ~300,000 women, so let’s learn about that next.
Maternal death
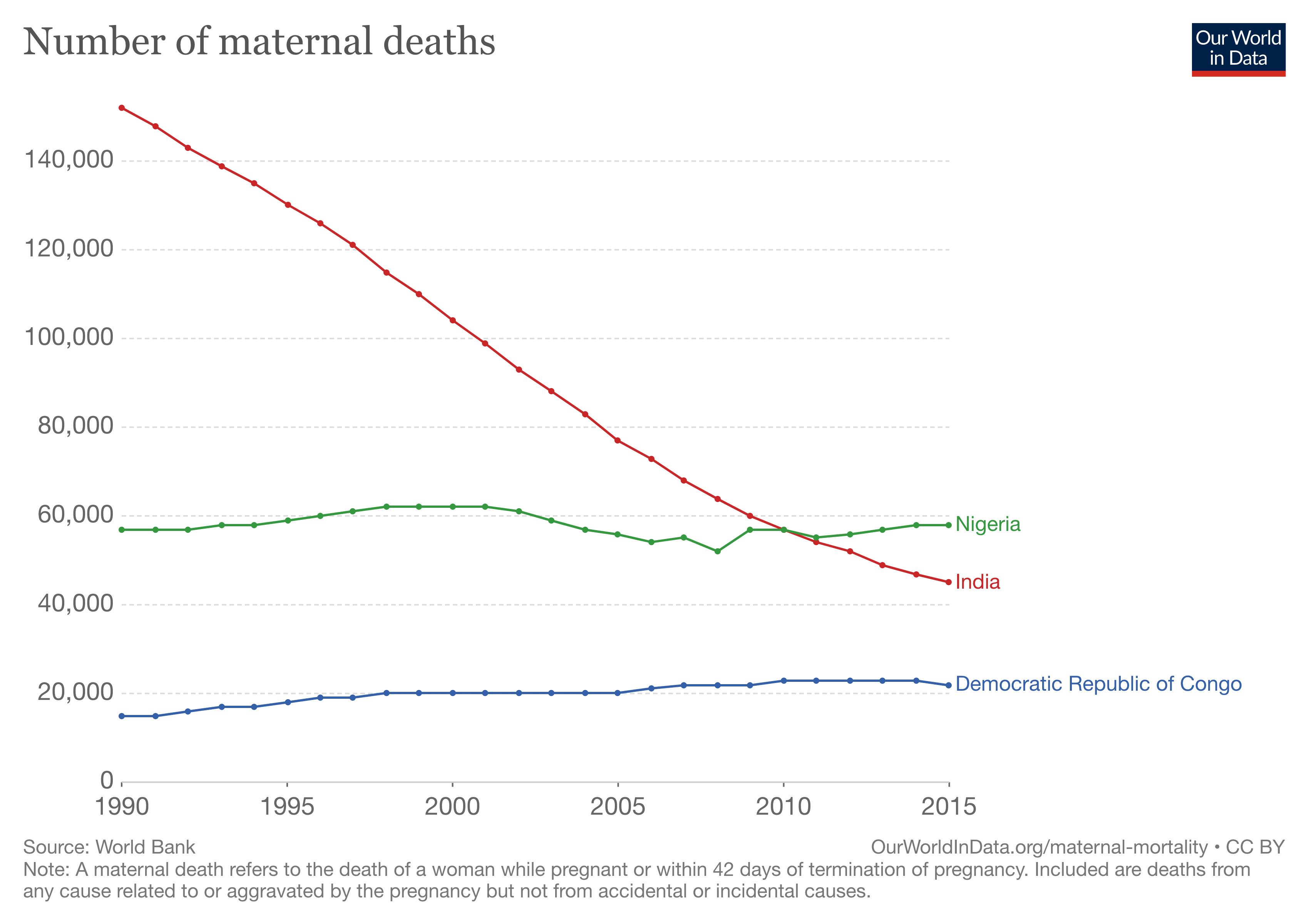
300,000+ women die from pregnancy-related causes / year. 66% occur in Sub-Saharan Africa, 22% in South Asia.
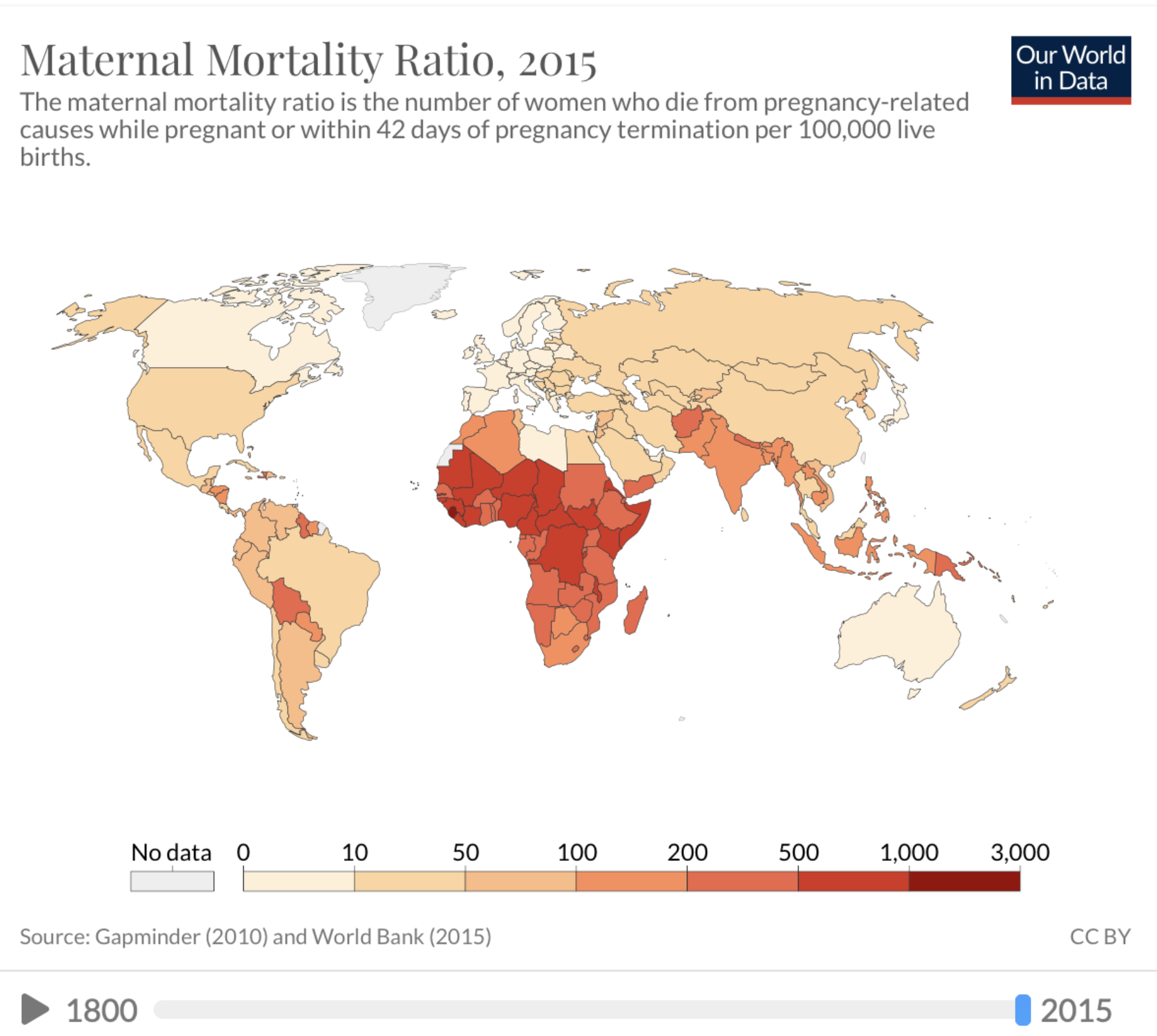
Reducing maternal mortality isn?t rocket science. Women didn?t always have smooth, easy births. But now, many western countries have less than 8 deaths / 100 000 births.
If the whole world had the maternal healthcare system of, say, Canada, we?d have 95% fewer maternal deaths. We would have 11,000 deaths instead of 303,000. We can do this with the information, technology and knowledge we have today.
It blows my mind that a woman in Sierra Leone is 450X more likely to die because of birth than a woman in Finland.
Most frightening: Africa has 2/3 of all maternal deaths, but it?s falling the slowest out of any place; at a rate of -0.95% per year. Compared to South Asia at -4.11%, East Asia & Pacific at -3.57% and Latin America at -2.70%.
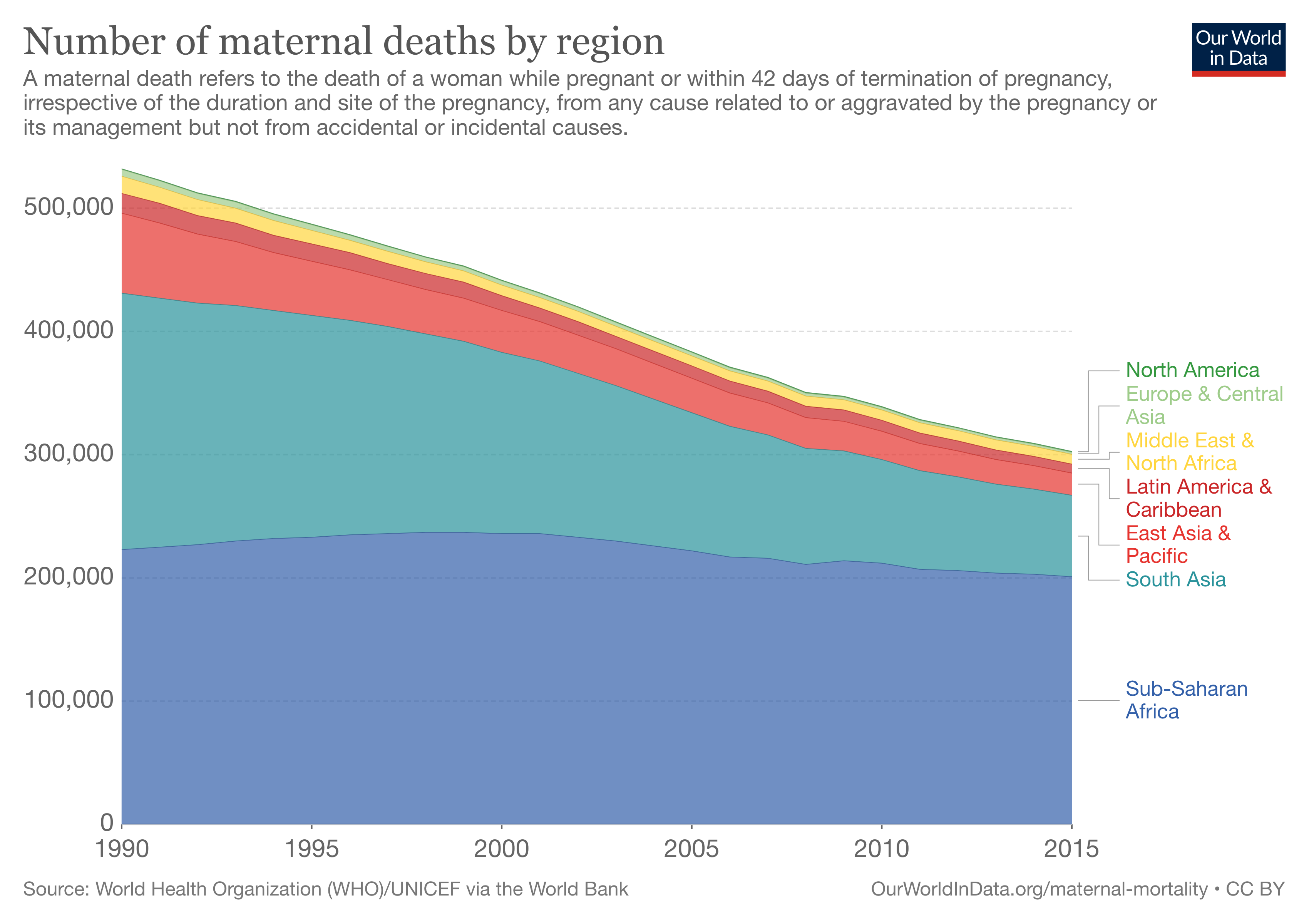 At the current rate of decline, it?ll take us 96 years to have 0 maternal deaths in Africa.
At the current rate of decline, it?ll take us 96 years to have 0 maternal deaths in Africa.
3 countries with the most maternal deaths: Nigeria(58k), India(45k), and The Democratic Republic of the Congo (22k). Solving these three countries would solve ~42% of the problem. India is the only country whose maternal mortality rate has a downwards slope.
What causes maternal death?
94% of maternal deaths happen in the developing world.
It?s not that we don?t know how to stop mothers from dying; we don?t have the resources to do so. Only 700 women die from maternal causes in the US per year; it is possible to get the maternal mortality rate down.
Unsafe Abortion: women in countries with illegal abortions still get them. They may drink poisons or use items like coat hangers to kill the fetus and remove it.
Severe bleeding: when women give birth, there can be a lot of ripping/blood involved. Pushing a 5?8lb object out of your vagina isn?t easy!! Thus, many women suffer from postpartum hemorrhages. Hemorrhages account for 27.1% of all maternal deaths. They?re the #1 maternal killer.

There?s even a mnemonic to remember the causes of hemorrhages! The 4 T?s:
Tone: lack of uterine tone (uterine atony). The uterus is the organ that houses the baby. It?s surrounded by muscle. After birth, the placenta detaches from the uterus, leaving behind blood vessels. Usually, the uterus deals with the blood vessels by ?contracting? them. But, the uterus can become ?too soft? to do so, which leads to bleeding.
 In the case of uterine atony, doctors will need to help it move.
In the case of uterine atony, doctors will need to help it move.
Trauma: Any damage to genital structures (vagina, cervix, so on). This type of bleeding can happen because of a stubborn baby, or medical equipment.
Tissue: the placenta normally separates from the uterus during labour. Yet, there are some cases where a part of that tissue stays attached. If this happens, it can lead to uterine atony (first T).
Thrombin: blood-clotting condition, where, clots can?t form. (It?s technically caused by a lack of thrombin doing its job). A small bleed can turn into a continuous bleed.
Infection: in the 19th century, 50% of mothers died because of sepsis. Then we learned to wash our hands.
Today infections cause 10.7% ? 15% of maternal deaths. But, we can reduce infection impact with good hygiene and antibiotics/antiseptics.
Some of the most common infections killing mothers are tuberculosis, pneumonia, group A streptococcus (GAS) and meningitis.
Hypertensive disorders: a group of high blood pressure disorders. They account for 7.4?14.1% of maternal deaths, and complicate 5?10% of pregnancies. Proven drugs like magnesium sulphate can help.
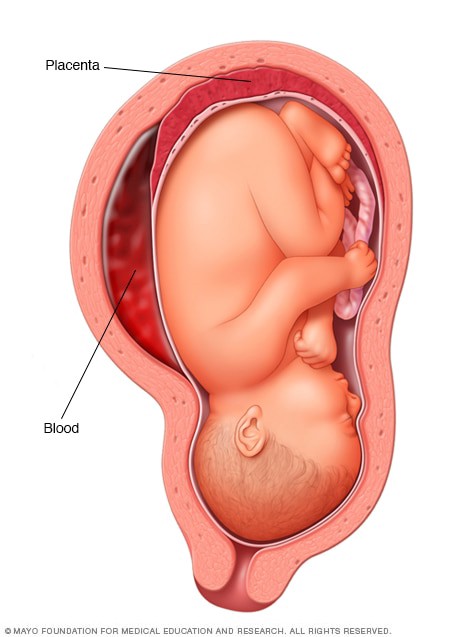
For pregnant women, preeclampsia is one of the most common disorders. It?s correlated to an abnormal placenta. The placenta has ?spiral arteries? which connect to the fetus. If these arteries are thinner, the fetus won?t have enough blood to develop.
If the placenta isn?t nourishing its child, it?ll release pro-inflammatory proteins. In short, these proteins narrow the blood vessels and makes the kidneys keep more salt.
This results in high blood pressure. With high blood pressure and restricted arteries, parts of the body will decline in function.
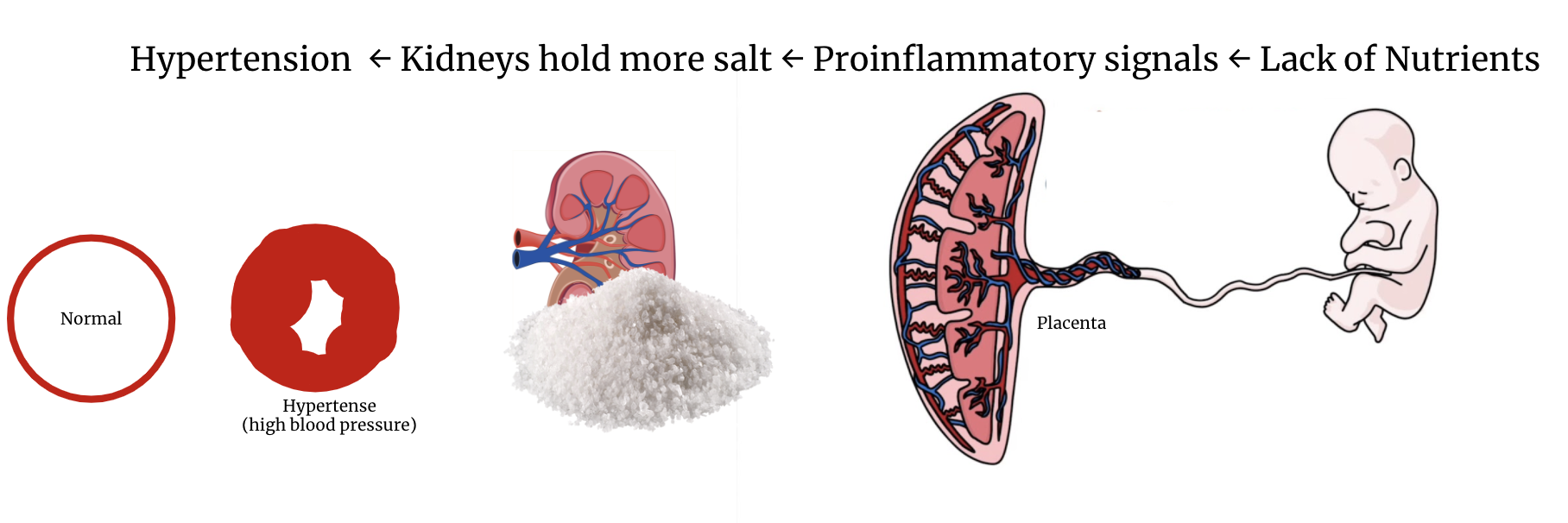
Sometimes, women experience seizures as well. If that happens, she has eclampsia. (Preeclampsia + seizures = eclampsia).
So, when the placenta behaves abnormally, the whole body gets affected. The placenta is like the foundation of a house; without it, it doesn?t matter what your windows or roof look like. You need that stable foundation.
Obstructed Labour: complications in how the baby exits the mother. Often, this means the baby will have less oxygen (and maybe die because of that).
Obstructed labour needs an operation to help deliver; like a c-section. In places with low-resources and unclean equipment, this exposes the mother to infections and trauma to her genital organs.
And that?s the high-level overview of maternal deaths.
Miscarriage
A miscarriage is when the fetus dies before it reaches 20 weeks of age.
15?20% of pregnancies end in miscarriages. Let?s take a second to let that sink in. ONE IN FIVE.
Why do they happen?
Chromosomal Issues
50% of them occur because of chromosomal problems. This is usually due to an extra chromosome/missing chromosome.
Every human has 46 chromosomes in most of their cells. These chromosomes contain all their genetic material. These cells have full sets of DNA, in biology, we call them ?diploid cells.?
There?s another type of cell with 23 chromosomes; these are your sex cells. Females have eggs and males have sperm. These contain 1/2 of your chromosomes, and in science, we call them ?haploid cells.?
No one is perfect, not even biology, so sometimes there are errors. Sex cells may have 22 or 24 chromosomes. This causes genetic problems during fertilization (when sperm + egg fuse).
Sometimes this results in a child with a chromosomal genetic syndrome. Examples are Turner Syndrome (45 chromosomes) or Down Syndrome (47 chromosomes)
Other times, the child doesn?t survive the pregnancy, and that?s when women have a miscarriage.
Cervix/Uterus competence
The cervix connects the vagina to the uterus. When it opens, it lets the baby out into the world.
Sometimes the cervix is too weak to hold the baby in. This can lead to premature birth or miscarriage.
Checking cervix status isn?t even a frequent part of prenatal care.
Age
The older a mother is, the ?lower quality of eggs? she has.
Her eggs tend to have more chromosomal defects. Women in their 20s have chromosomal defects in 17% of her eggs, women in their 40s have it in 79% of their eggs.
Women age 45+ have a 53% chance of miscarrying.
From the lens of evolution, this makes sense. A younger woman has more years to live and care for her child than an older one. So, a woman will ovulate her best eggs first.
Other potential reasons
We often associate miscarriages with ?uncontrollable causes? ? like chromosomal errors.
It?s the wrong mindset to have. We?re never going to change the status quo if we accept it.
But, scientists have started formulating other hypothesizes.
- Infection. Some infections/viral diseases impact pregnancies, others don?t. We?re not sure (shocking), but we are studying it.
- Hormonal Imbalance. Ah, so we meet again. Science is investing the correlation between miscarriage and LH, Progesterone, FSH , antimllerian hormone + more.
- Thyroid autoimmunity; see this study.
We have our theories, but we still can?t explain the cause of around 50% of miscarriages. Luckily, around 3/4 of those women go on to have normal pregnancies. I still find it crazy how we have not uncovered preventative measures for miscarriages.
In the world, we have around 130?140M births per year. If we?re conservative with numbers, around 19.5M fetuses die due to miscarriage (130M * 0.15).
Still Birth
If a fetus is not alive after 20 weeks, it?s considered a stillbirth. We call this ?pregnancy loss? ? not miscarriage.
There are 2.6M stillbirths globally. These babies are born dead.
Why does it happen?
Problems with the placenta.
25% ? 50% of stillbirths happen because of placental issues.
The main job of the placenta is to support the vulnerable baby. It can?t feed itself. It can excrete on its own. It needs help, and that?s what the placenta does ? through the umbilical cord.
The placenta is the passageway between the mother and child. It?s attached to the outer layer of the uterus, aka the endometrium. There are layers of blood vessels within the endometrium. This is crucial to supplying the placenta with resources for the baby.
The placenta has 5 functions:
- ?Respiration; replicate the lungs
- ?Excretion; replicate the kidneys
- ?Nutrition; replicate the digestive system & nourish the baby
- ?Immunity; provide antibodies
- ?Hormones; produce hormones to keep the pregnancy healthy. The main hormones are HCG, estrogen and progesterone.
I like to think about the placenta as a refrigerator, and the baby like a carton of milk. The milk needs the refrigerator for support. The fridge provides the milk with everything it needs; a place to stay and temperature between 38 and 40F.
If the milk leaves the fridge for more than 2 hours, it will go bad.
When is the placenta a poor fridge?
- When it doesn?t give the milk what it needs. It might be too hot or too cold. This doesn?t spoil the milk completely but ruins it slightly.
- When it shuts off completely.
I don?t know about you, but I personally like when my fridges are cooperative.
So does your baby. It can?t survive without its placenta.
What are the ways the placenta can turn down the temperature or shut off?
Placental Abruption: the placenta detaches from the uterus prematurely. This happens after birth in most cases; when the baby is already out. Removing the placenta is the ?3rd phase of labour.? Yet, if this happens too soon, the baby will get less support than normal, which may hinder its development.
Abnormal (velamentous) cord: connects the baby and placenta in an abnormal way, which impacts its function.
 Cord wraps around baby
Cord wraps around baby
Umbilical Cord problems.
This impacts 1 in 10 stillbirths.
Recall from 20 seconds ago; the umbilical cord connects the baby to the placenta.
It can be nourishing, but it can also be dangerous.
How does the baby die? The cord gets knotted/squeezed around the infant, which cuts off their oxygen. Or, the cord gets damaged which stops the supply of oxygen/nutrients.
No oxygen = no breathing. Every human needs a little O2.

Infections
This impacts 1 in 10 stillbirths. Some studies bring that number up to 1 in 4.
There?s 130 bacteria that cause infection in the uterus, and ~1/3 have good evidence for correlating to stillbirths. There are 43+ bacteria that can invade the genital area of a pregnant woman and kill her child.
When these bacteria enter the uterus, they can affect the amniotic fluid. This is the fluid that surrounds the baby, helps keep it in place and gives it important resources.
If a baby has too little or too much fluid, it could be in serious trouble. We want to keep the level at ?average,? but we also want to ensure the fluid is healthy. Invasive bacteria don?t do that.
Viral infections can also spread to babies; like the Coxsackie virus.
Birth defects
This impacts 1 in 10 stillbirths.
If the baby has developmental or birth problems, they?re likely to have problems during pregnancy. Sometimes this means not making it through the pregnancy.
What are some of the most common ways this happens?
- We?ve talked about chromosomal problems in miscarriages, but it still remains true here. Genetic disorders like down syndrome increase the risk of stillbirth.
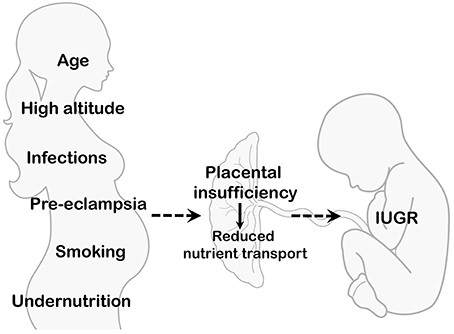
- Intrauterine growth restriction is when the baby grows slower than it should be.
Other potential causes
- Maternal medical conditions. The mom is housing the baby; if something is wrong with her, it can danger the child. This impacts <10% of stillbirths.
- High blood pressure disorders (like preeclampsia mentioned in the maternal death section).
- Labour complications. Such as preterm labour, carrying more than one child or prolonged pregnancies (42 weeks+).
- Lifestyle. Smoking, drugs, and dangerous substances kill babies.
- Or, it might remain a mystery forever. One study found that 25% of stillborn cases are unknown.
What?s the femtech opportunity?
We?ve talked a lot about the ?death? behind pregnancy.
It?s a difficult task for someone to make a human. There are many things that could go wrong. But here?s the important thing: constantly checking up, to make sure things go right.
Many women avoid these challenges through high-quality prenatal care. Having your doctor check up on you, and the baby ensures everything is running along.
We need more of this, especially in places that don?t have easy access to prenatal care. Lack of prenatal care is associated with 40% higher neonatal mortality (death of your child within the first month of life).
Better and more scalable prenatal care.
This includes:
- More vital tests.
- Digital care: more things to do at home.
- Ways to avoid miscarriage, stillbirth and other pregnancy risks.
To be honest, we have too many ?unknowns? in these situations. We don?t know most causes of pregnancy-related, or women?s health-related problems. What if we knew more?
Have more skilled staff at hospitals; and better resources.
Considering that many of these problems happen in the developing world, it?s clear this isn?t only about ?science.? Sure, we don?t know a lot about why many of these happen.
But, a woman in the Democratic Republic of the Congo should have the same chance at a healthy family as one in Australia. This is about democratizing a system that already exists.
Ways to provide better contraceptives or safer abortions.
Sometimes it?s not the right time for pregnancy. Making abortion illegal doesn?t decrease the desire for abortion. If we make contraceptives better, we?ll need fewer abortions. If we make abortion safer, fewer women will die from dangerous abortions.
Giving Birth
When the baby reaches 37?42 weeks of gestation, it?s ?cooked enough? and ready to enter the world.
Gestation is the number of weeks since the first day of the woman?s last menstrual cycle. Not conception.
How does birth work?
Let?s talk about ?natural? or vaginal birth first.
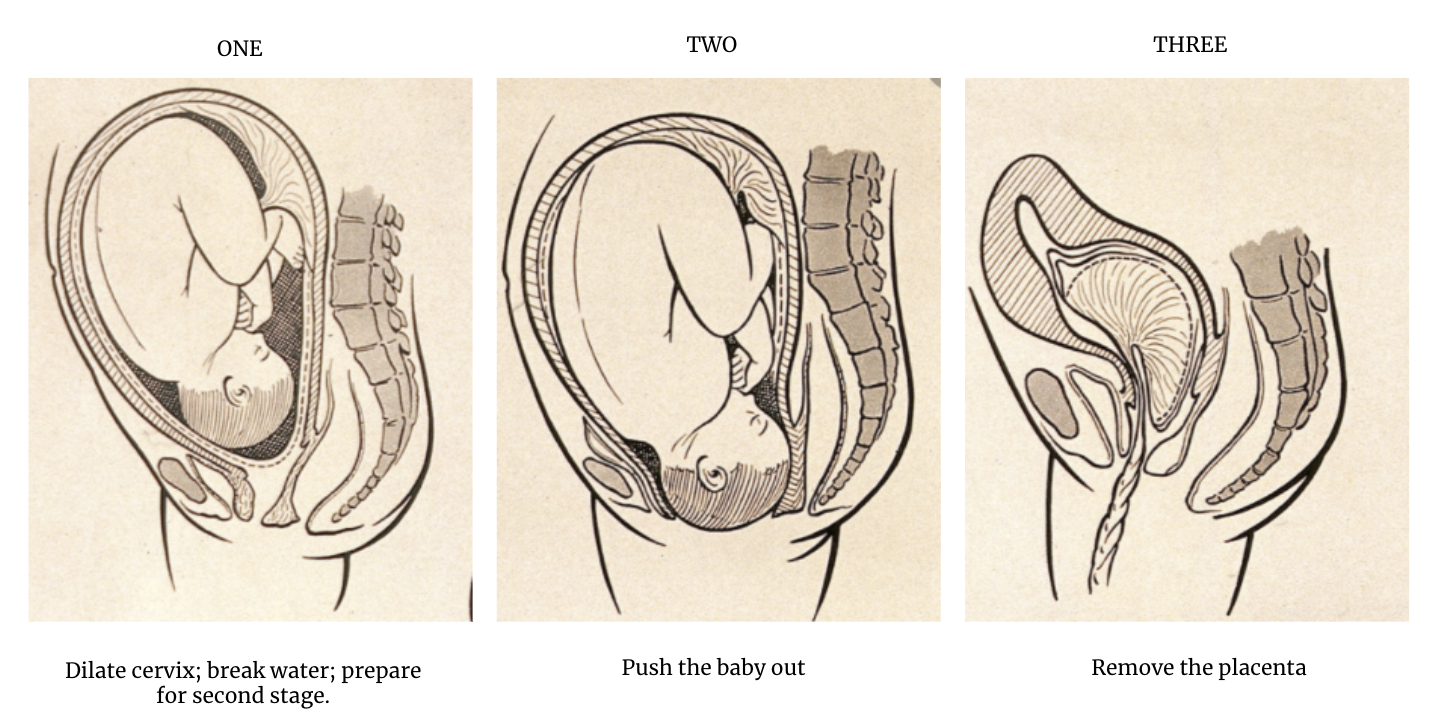
Women go through 4 stages of labour.
- Contractions start; what breaks; the cervix dilates to 10 cm.
- Baby moves through the birth canal (vagina) and gets born.
- Uterus contracts to remove the placenta. Happens ~5?15 mins after birth.
- Postpartum recovery; first 6 weeks after birth.
?Let?s have a closer look at these steps.
1-Opening the cervix
The cervix sits between the vagina and the uterus.
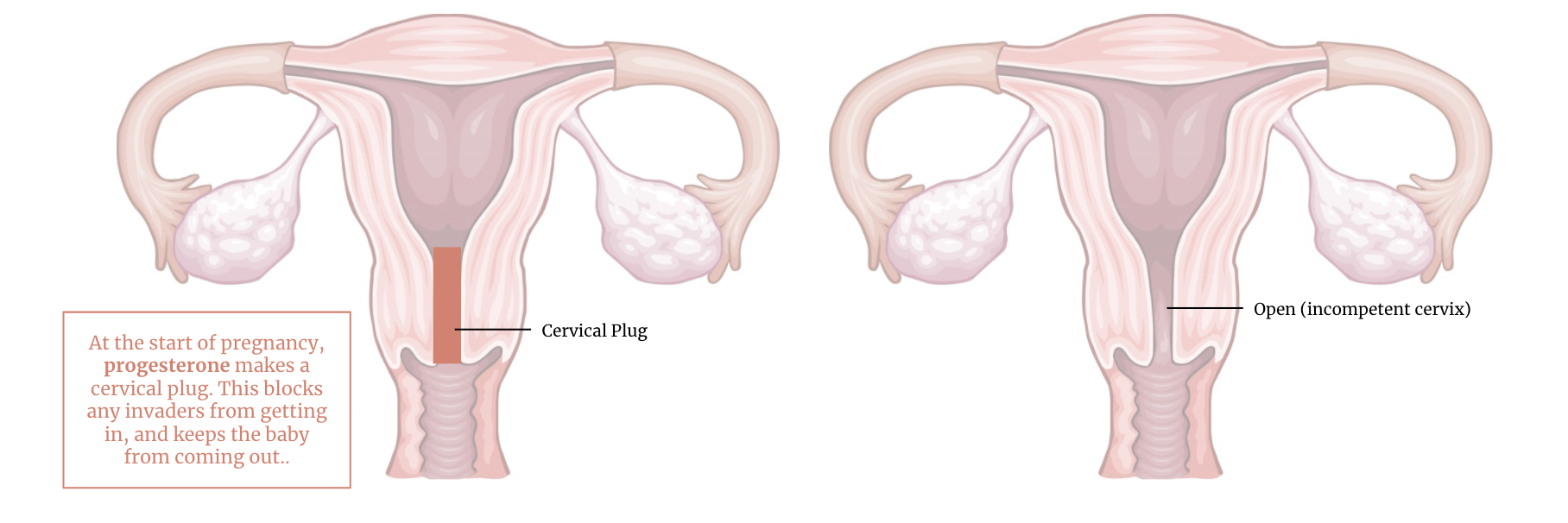
During pregnancy, the body produces a thick cervical mucus that acts like a plug. This plug protects the uterus/baby from any infections or foreign invaders. Not to mention, it keeps the baby inside.
The cervix is in charge of keeping the baby inside and letting the baby out when it?s ready.
During labour, the first step is opening the cervix. We consider it fully open when it?s 10 cm in diameter.
How does this happen?
Hormones ?.
During labour, hormones do 4 things:
- Signal to the mother that the baby is ready for birth
- Start uterine contractions to push the baby out
- Dilate the cervix
- Prepare mother for nursing (breastfeeding)
In this section, I?ll focus on #1?3.
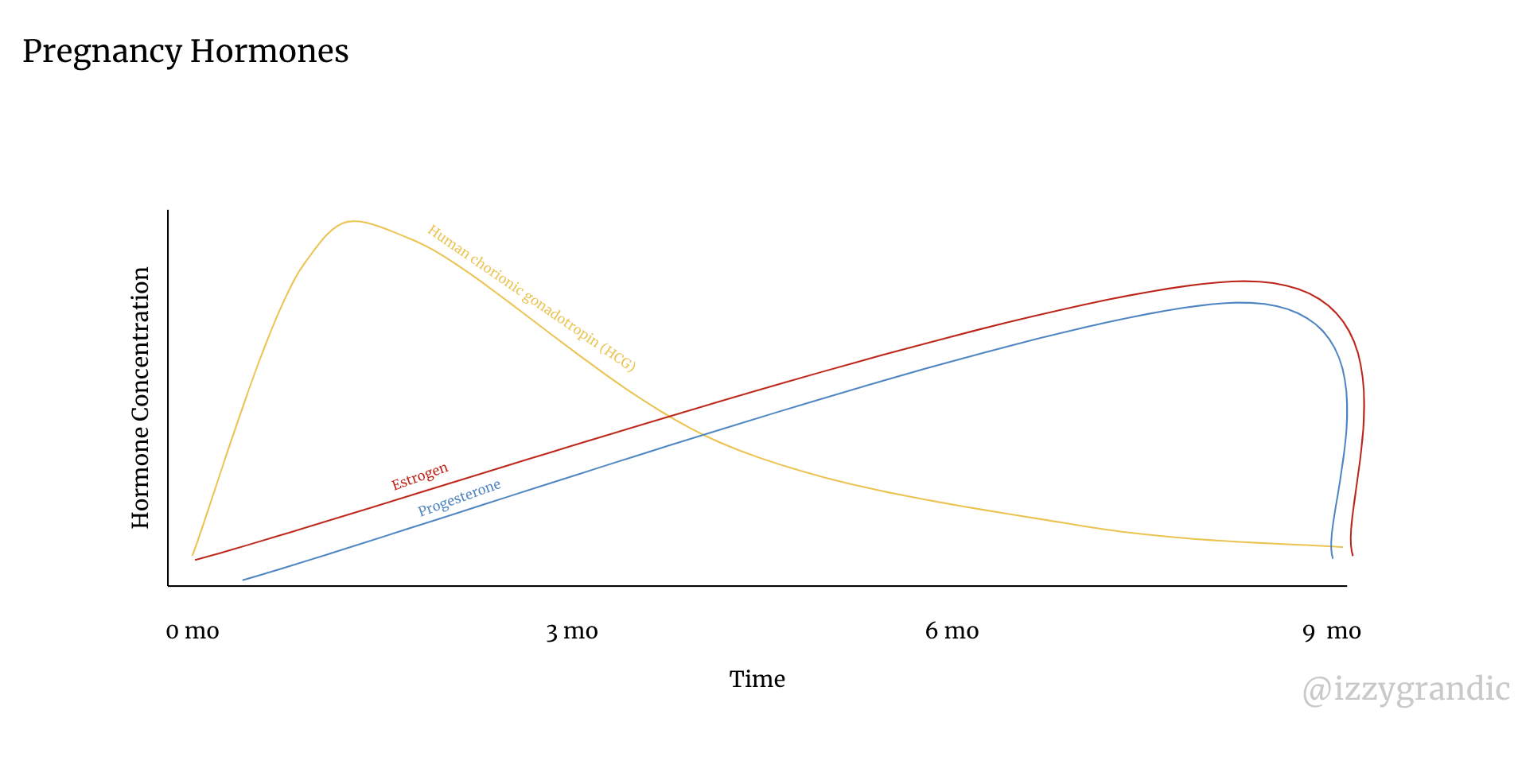
During the 9 month pregnancy, hormones are preparing the body for birth. There are 3 main ?pregnancy? hormones: HCG, Estrogen and Progesterone.
This is how the 3 hormones change over the course of fetal development.
- Estrogen increases the number of oxytocin receptors (you?ll see why this is important in a sec)
- Progesterone relaxes the uterus and stops it from contracting. This lets the baby grow, and stay inside. During labour, when we want the uterus to contract, we need to decrease progesterone.
?Signalling Birth
When the baby reaches its maximum size, it causes pressure on the reproductive surface. The fetal stress then signals special cortisol (stress) hormones like corticotropin.
The increase in stress hormones tells the body to start getting prepared for the big show.
After the cortisol release, there are 3 main hormonal changes:
- Decreased Estrogen
- Decreased Progesterone (which un-softens the uterus so it can start contracting)
- Increased Prostaglandins (kick starts uterine contractions)
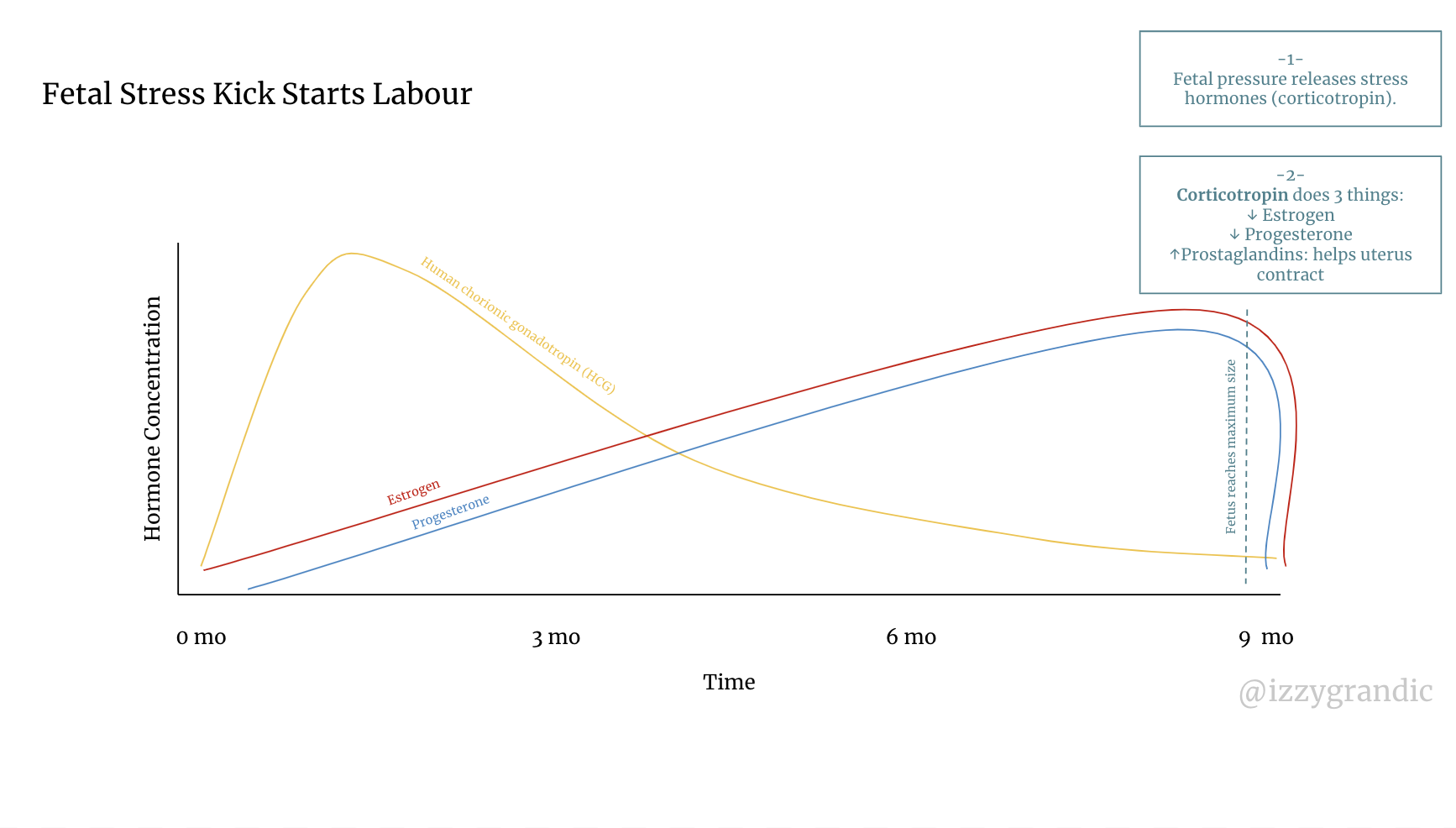
This cocktail of events gets the uterus contracting. Theses contractions continue to add pressure, which releases more hormones to help contractions. It becomes a cycle of many contractions that become intense over time, leading to birth.
Specifically, the prostaglandins and oxytocin fuel contractions and cervical dilation. They work through a positive feedback loop.
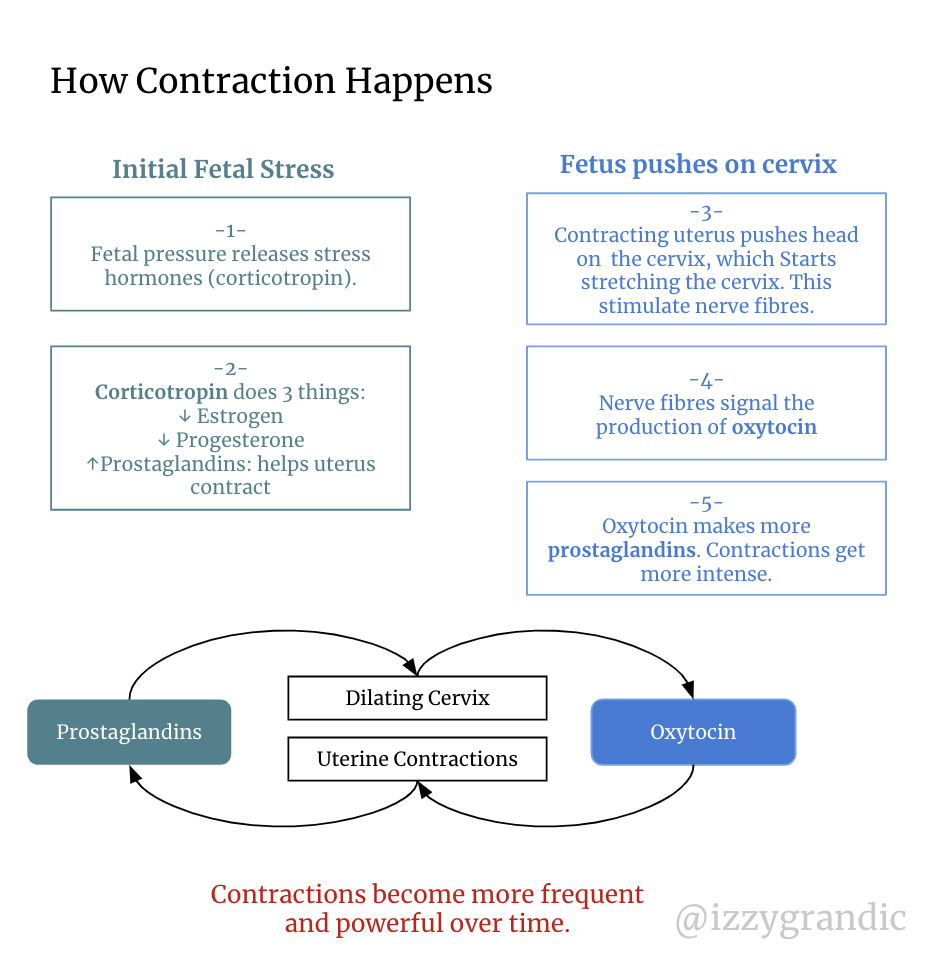
As contractions start to pile up, the body also releases relaxin. Relaxin, as the name suggests, ?relaxes? the lower pelvic region, to help with a smoother delivery.
This combo of cervical dilation + contractions does two other things:
- Ruptures the amniotic sac (commonly referred to as ?water breaking).
- Removes cervical plug (made of thick mucus).
The whole process to go from 1?10cm dilation of the cervix will take ~8?16. The cervix goes from the size of a cheerio to the size of a melon. ?
For more on labour hormones, I?d recommend this reading.
2-Push that Baby!
There are two things that need to happen to deliver the baby:
- The cervix needs to fully dilate (open to 10 cm diameter)
- The uterus needs to continue contracting
Once the mom has an open cervix and a contracting uterus, she?s ready to push that baby out!
How does this happen?
- The mom has her ?flight or fight hormones kick in. These give her the big ?push.? Epinephrine (adrenaline) and norepinephrine (noradrenaline) are the hormones that get activated.
- She?ll start pushing the baby. The uterus is a muscle, and it will be very very tired/painful during this phase. It?s working hard. ?

- Sometimes the mother will push too hard that she tears the perineum (skin between the anus and vagina). Sometimes, the midwife/doctor will cut the perineum to ease the passage of the baby. This is an episiotomy.
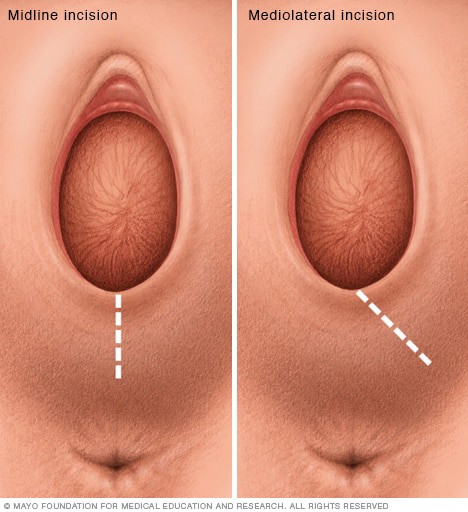 An episiotomy helps the baby ?slip out?
An episiotomy helps the baby ?slip out?
Once the baby is out, the very hard part is over. Next, we cut the umbilical cord and bring the baby to the mother, unless there is a health concern with the baby.

3-Removing the placenta
Once we deliver the baby, we no longer need the placenta.
Before the mother can embark on postpartum recovery (bringing her body back to ?normal?) she needs to expel the placenta.
It?s a similar ?process? as giving birth. The uterus contracts and the placenta gets pushed through the cervix. Except, there?s less build-up, and less ?hype? at the other end.
 Placenta (front) baby (back)? if you couldn?t tell.
Placenta (front) baby (back)? if you couldn?t tell.
But how exactly does this happen?
- Oxytocin is back at it! It continues contraptions post-birth to help remove the placenta.
- Your birth provider may give the mother an injection to amplify contractions. After a long, difficult birth, the uterus may be very tired. The midwife/doctor injects syntocinon or ergometrine (drugs) into the mother?s thigh.
?And that is how to deliver a vaginal birth.
What if a woman can?t give a vaginal birth? Welcome to the c-section.
A few weeks ago I was in San Francisco. I just landed at SFO, and I needed to get to Berkeley.
In light of being a broke student, I decided to take public transit, aka 7 buses, to get where I needed to go. (To be fair, I made a detour to go to Lombard Street, so I overcomplicated my route).
Carrying a 40-pound suitcase made my whole public transit adventure less thrilling. 5 buses and a donut later, I was at West Oakland station calling an uber.
I gave it a shot. I had an adventure, and I enjoyed it. But I didn?t finish it; I had a more attractive, less adventurous option: uber.
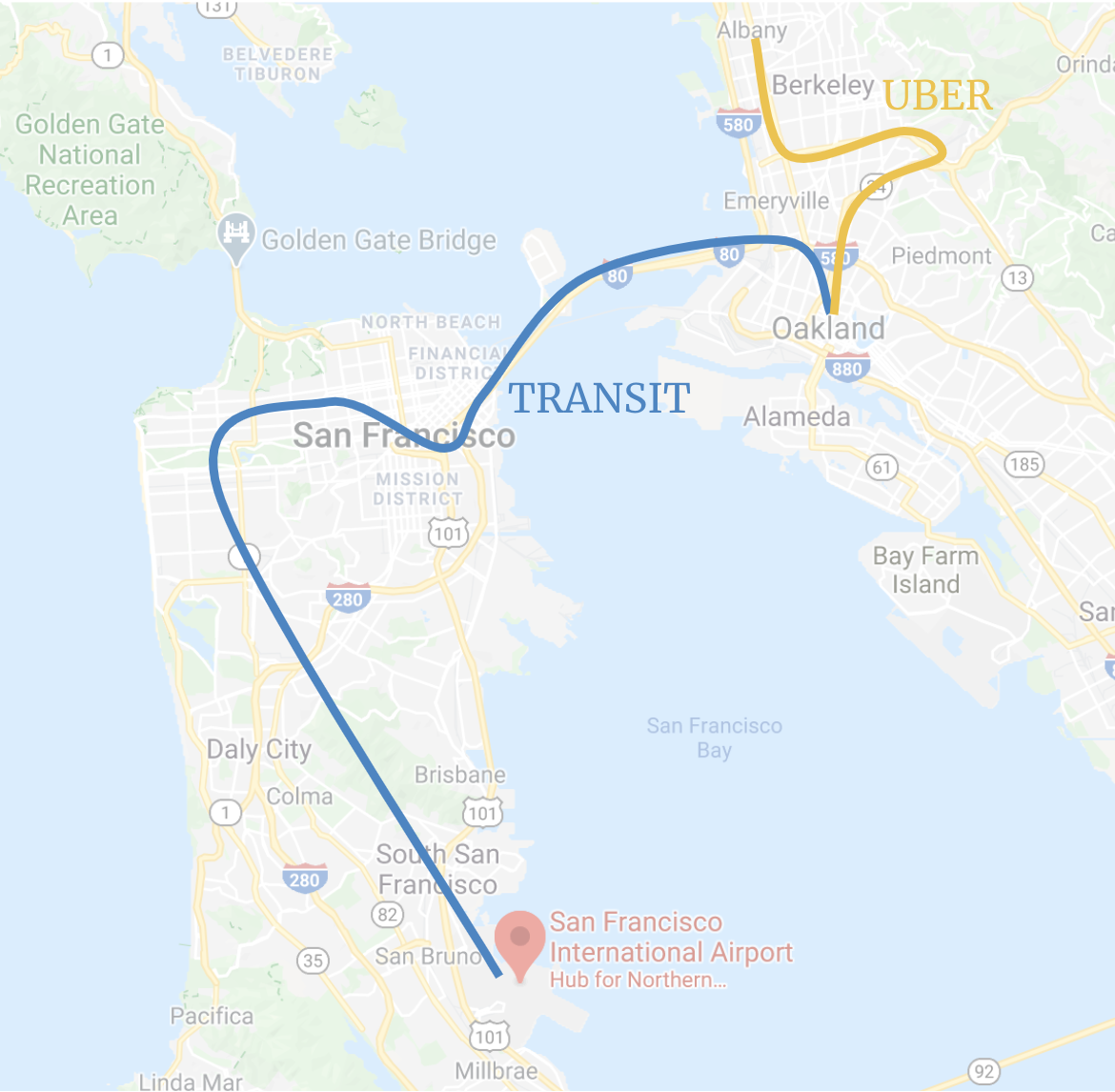
C-sections are the uber for childbirth.
It?s a 45-minute major abdominal surgery that literally cuts to the chase.
Now, getting real here, ?C-sections? are actually called ?Cesarean sections.?
There are a 4 ?medical? reasons mothers get a c-section:
- Placenta Previa: When the placenta blocks the cervix. The baby can?t get out.
- Fetal Distress: when the health of the baby gets compromised. If the fetus is in danger, we may need to deliver it quickly. Multiple births increase the odds of fetal distress.
- Baby can?t fit through birth canal: sometimes heads are too big, or the baby is in an unfavourable position.
- Compromised maternal health: diabetes, tumours, infections, etc.
How does the c-section work?
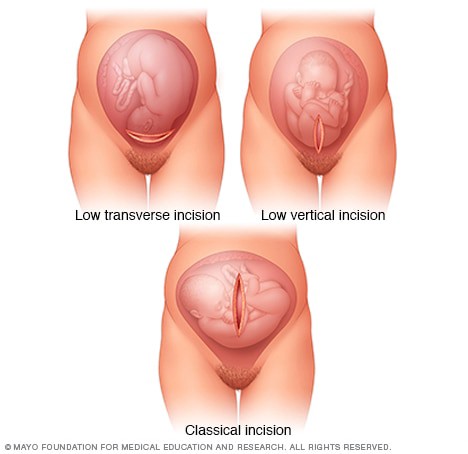
Step 1: An incision.
The doctor cuts horizontally/vertically on the abdomen and the uterus to access the baby.
Step 2: Rupture & Remove.
A membrane surrounds the baby, which keeps the amniotic fluid inside.
In a vaginal birth, the mother?s ?water breaks? before she gives birth.
During a c-section, doctors rupture the membrane (?breaking the water?) and deliver the baby.

It isn?t rocket science; the doctors pull out the baby. Sometimes there?ll be complications with the baby (especially if it?s an emergency c-section). The baby may require some followup examination/procedure.
Step 3: Chop the umbilical cord and remove the placenta.
Like in a vaginal birth, we must detach the baby from the umbilical cord; the steps aren?t different.
To get rid of the placenta, the doctors just pull it out.
Step 4: close.
Tightly suture the abdomen and uterus. Now the surgery is complete! Doctors will hospitalize mothers for a few days (3?5), and they will recover in 6?8 weeks.
HORRAY!
 C-section incision
C-section incision
C-sections have decreased maternal mortality global morality. They?re an awesome emergency option.
But, they only decrease mortality up to a certain point. When % of c-sections reaches 19%, benefits for mothers and children disappear.
1 in 3 women in the US get c-sections. Only ~1 in 10 needs them. Women aren?t having safer births, they?re having more unneeded major surgeries. Why? It could be that doctors get paid 50% more to do a c-section.
Nonetheless, c-sections have impacted maternal and fetal mortality. And it?s settling to know women have other options to safely deliver.
Now, this whole birthing process isn?t cupcakes and roses. It can hurt, a lot. What are the ways women giving birth can manage the pain of pushing a human through a 10cm hole? Or having major surgery?
There are non-drugged approaches like meditating, listening to music or taking a bath. These are more understood, so I?ll focus on the medical approaches.
Medical approaches.
We have two varieties of medicine for labour:
- Analgesics: reduce pain, but not entirely
- Anesthetics: numb your entire feeling.
Labour-activities deal with the waist and below, so these medications act on the bottom half of the body.
Time to get down into business: what are the different types of pain medication?
- Epidural; they ?freeze? your lower back. It?s a procedure that sticks a needle in the mother?s back with a catheter. We use the catheter to re-administer pain meds when needed. This is important because vaginal childbirth isn?t a speedy process. Mothers might need an extra dose every few hours. When administered, it takes ~30mins for an epidural to kick in.
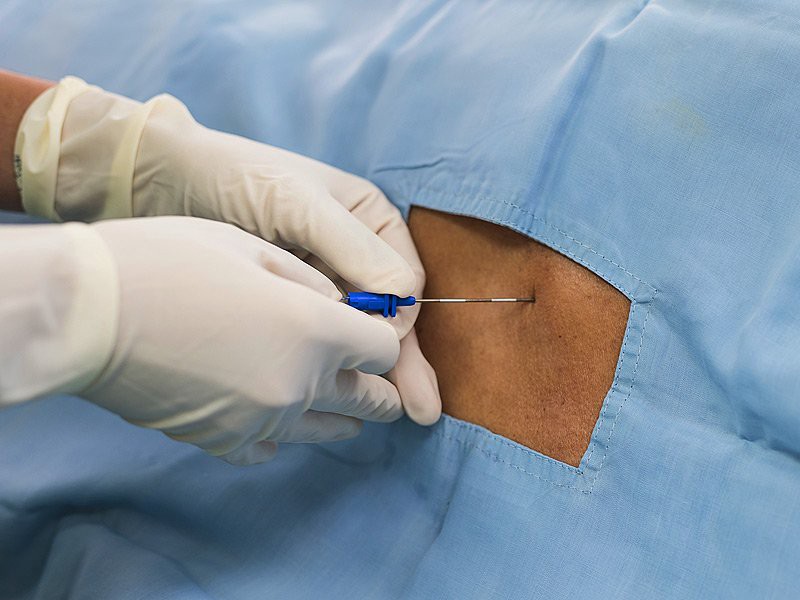 Epidural
Epidural
- Spinal block (mostly used for c-sections). It?s an injection in the lower back that works like an epidural. But it works almost immediately and is short-lived. Luckily c-sections only take ~45 minutes; vaginal births can take 20+ hours.
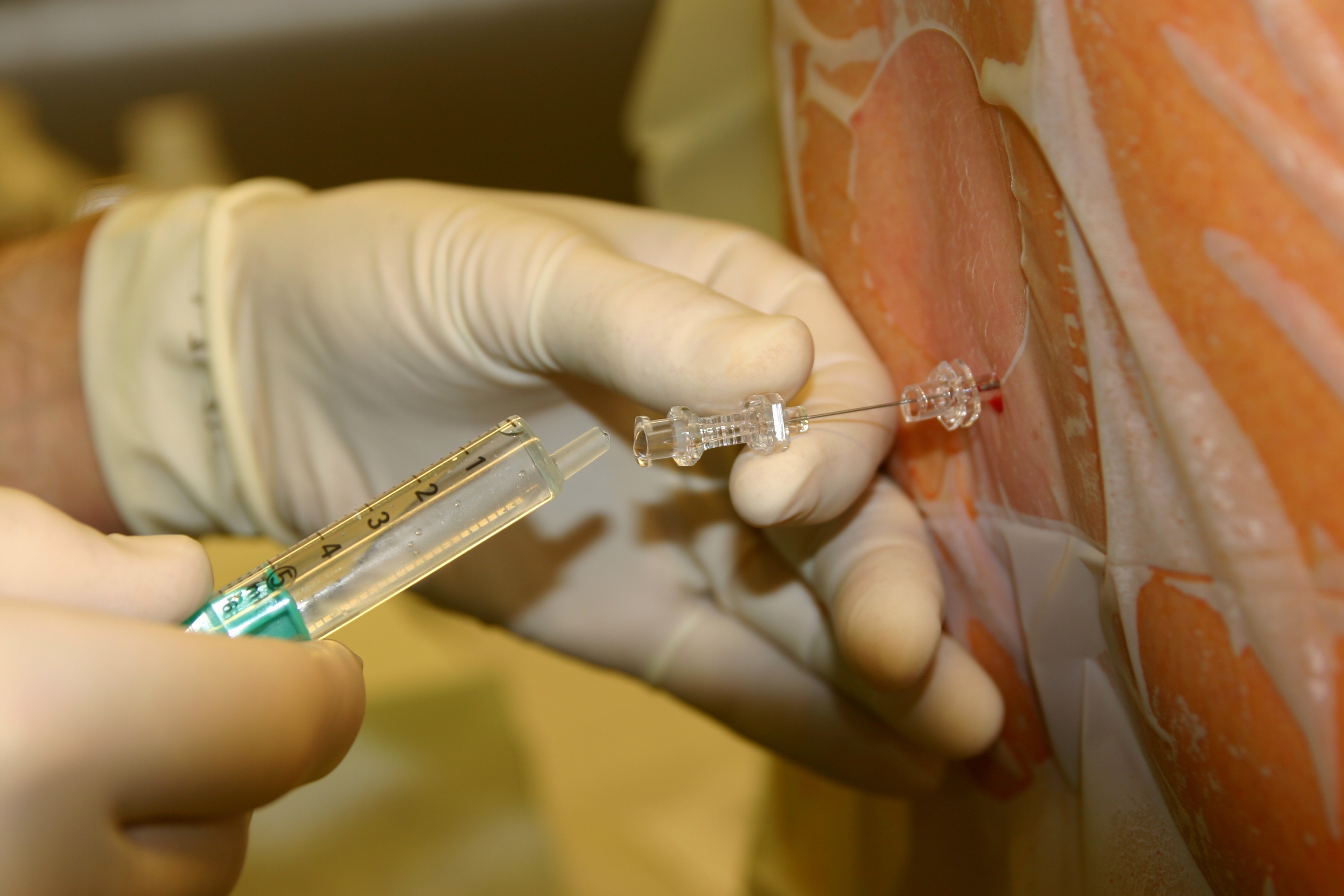 Spinal Block; think of it like a temporary epidural.
Spinal Block; think of it like a temporary epidural.
- Combined spinal-epidural (CSE). It?s a combination of epidural and a spinal block.
- Pudendal block. Injections in your perineum (the area between anus and vagina) to ease the pain. Generally, childbirth puts a lot of pressure on this part of the body.
- Narcotics (opioids). Beyond initiating a crisis, we can use opioids to lessen pain for 2?6 hours.
- Drugs through intravenous (IV) administration. A woman can receive a series of pain killers, like tranquillizers, through IVs. They don?t block out all the pain, but, they offer some relief. Like how advil doesn?t solve all your problems, but holy moly it is helpful.
To recap: on the medical front, there are two classes of options.
- Inject anesthetics to stop pain from happening, Epidural, Spinal block, etc are all different techniques.
- Administering drugs/pain killers.
The length of time a baby stays in her mother before birth is important.
Babies are like cooking turkeys. It?s possible to undercook it or overcook it. Both are bad. You should aim to regular ?cook? your turkey.
Anytime before 37 weeks is premature. There are different levels of prematurity:
- <28 weeks: extremely preterm infant
- 29?33 weeks: preterm infant
- 34?37 weeks: late preterm infant
About 11.4% of babies in the US are born too soon. Globally, preterm births contribute to 1M deaths among children under 5. It?s the single biggest cause of infant mortality. 15M babies are born prematurely around the world.
Anytime after 42 weeks is post-term. This impacts 5?10% of pregnancies and can lead to induced pregnancy.
Induced pregnancy is when we use artificial methods to kickstart delivery. Sometimes, women need the extra push. In particular, 23?33% of the time.
 Induced labour (left) taking over regular labour (right).
Induced labour (left) taking over regular labour (right).
There are many ways we can induce labour:
- Stimulating the cervix to release prostaglandins. To do this, your doctor/midwife makes circular movements around your cervix with their finger.
- Injecting synthetic prostaglandin. This softens the cervix and is more effective than stimulating the cervix.
- Cervical ripening balloon catheter. Insert tube + balloon into the cervix to non-hormonally cause it to open.
 The balloon catheter adds extra pressure and starts stretching the cervix.
The balloon catheter adds extra pressure and starts stretching the cervix.
- Injecting synthetic oxytocin (Pitocin). This hormone helps start contractions to push that baby out.
- Rupturing the membrane; i.e., breaking the water. There?s a thin membrane that holds in the amniotic fluid.
Because induced labour is ?unnatural,? there are several downsides to it.
- 25% of the time it doesn?t work.
- It can make contraptions too strong, which can damage the baby?s heartbeat.
- It can cause fetal & maternal stress.
- More painful labour, that?s more difficult to manage.
- More likely to need an epidural.
- If a baby wasn?t ready to exit; it can cause health concerns down the line.
Induced labour is like buying toilet paper during a pandemic (like COVID-19). It?s intense, excessive and driven by fear. There?s extra stress added to a simple task.
But, during non-pandemic times, buying it isn?t that anxiety-prone.
Today, many women are inducing their labours out of convenience and scheduling. They want to speed up the process. They want to be more ?prepared.? In most cases, this is bad for both the mother and the fetus.
Sometimes, you don?t need heaps of toilet paper in your basement, and sometimes you do.
?The exact events leading up to the onset of labour are still not fully understood.? Yup, this is yet another area in women?s health we have so much room to explore.
Postpartum recovery.
To grow a human, the body changes a lot.
After birth, when there?s no human left, the body needs to return to its normal state.
This recovery can last up to 6 months and it?ll vary based on your birthing method (vaginal vs c-section).
Beyond physical adjustment, women experience extreme mental/hormonal adjustment.
In this section, I?ll go over the 3 types of postpartum recovery:
- Vaginal
- C-section
- Mental Health
Let?s! Get! Started!
Vaginal
Imagine doing a 24-hour high-intensity workout? that?s basically what the uterus goes through during birth.
Whenever I do a tough workout, I feel the soreness for days. Pregnancy is like the most intense workout of your life, amplified by 1000, in the most sensitive area of the body.
TLDR: It hurts to do anything down there after birth ? for weeks or months.
In the first few weeks, women are often:
- Very sore; hurts to walk, sit, or do anything.
- Bleeding. A lot. This can last ~6 weeks.
- In pain due to the uterus contracting. During pregnancy, the uterus expands to 500?1000X its original size. It takes about 6 weeks to return to pre-pregnancy size.
- Not in control of their bladders. Muscles are loose; it?ll be difficult to go to the bathroom.
How do we recover?
?Wait it out.
????Maintaining a healthy lifestyle.
?Use post-partum products to make your life down there easier. Some examples:

C-section
A c-section?s recovery is much like any major surgery. At first, the incision will hurt, and it might be difficult to move.
Women who had c-sections still go through a contracting uterus ? but that?s most of the pain ?down there.?
Women with c-sections need to:
- Protect their incisions and let them heal while avoiding infection.
- Get through the uterus-shrinking cramps.
- Take precautionary measures to avoid blood-clots ? like taking heparin. After childbirth, the body discharges its extra tissue/blood from the pregnancy. Women who had c-sections were 4X more likely to develop blood clots.
This process said to take 6?8 weeks, but certain studies found that 60% of women felt pain in their incision point 24 weeks later.
Mental health
85% of women experience some mood disturbance. The culprit? Hormones.
Chemicals in the body and brain change rapidly. Which causes women to go through the ?baby blues? and/or ?Postpartum depression.?
Without slapping an endocrinology lecture in your face, let?s quickly look at the hormones.
During labour, estrogen & progesterone plummet. Stress-related hormones, cortisol, ACTH and corticotropin increase quickly.
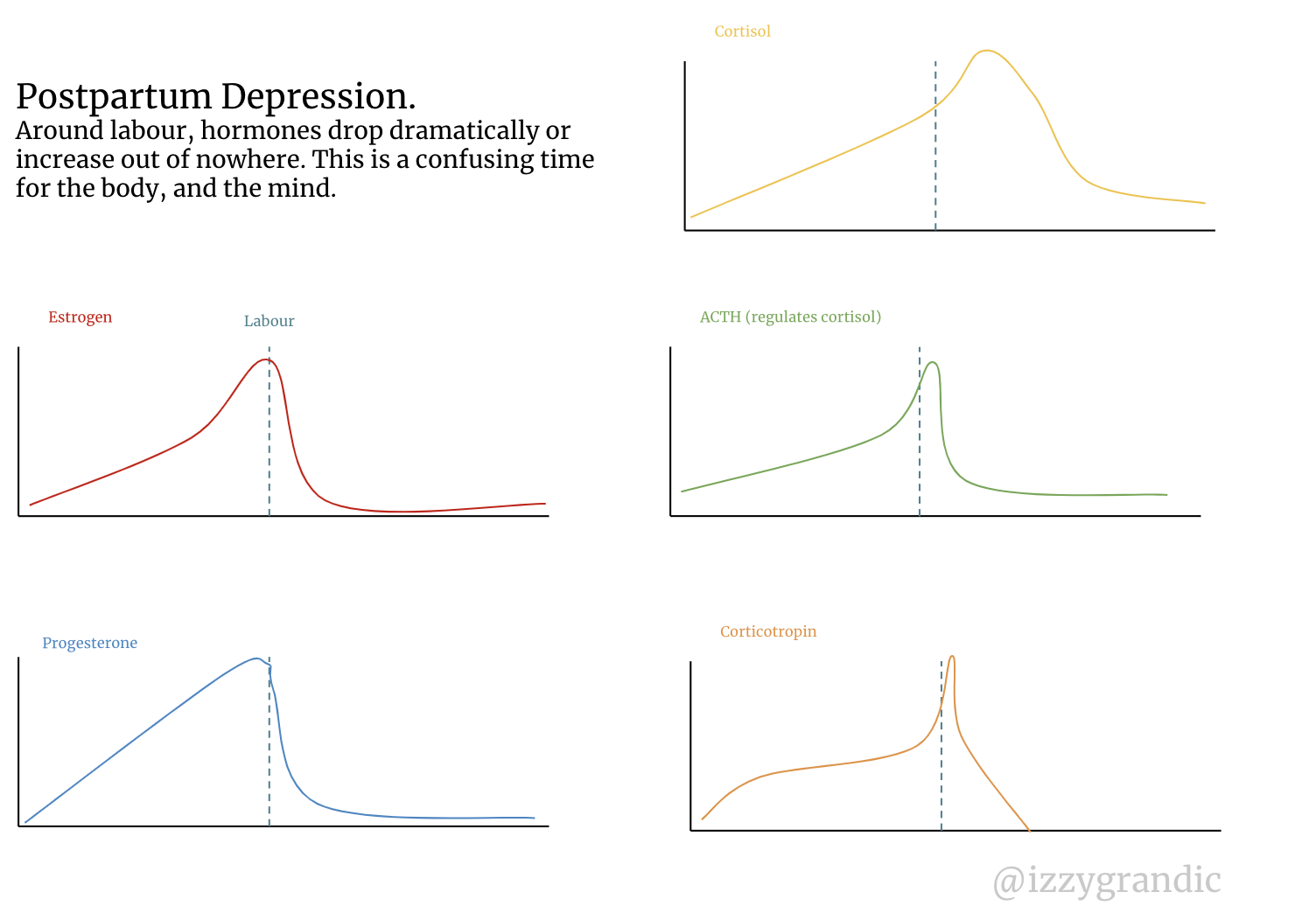
This is a HUGE area that?s underfunded, unexplored and impacts tens of millions of women. To learn more I recommend this source and this article I wrote about postpartum changes.
Breastfeeding
Throughout most of a girl?s life, breasts are just ?there.? But after birth, it is their time to shine. Party time ?.
The purpose of boobs is milk production. This milk production gets stimulated *when you have a baby*.
I know, I was getting excited about having an unlimited milk supply on my chest to cut my dairy costs too. But, to lactate *generally* women need to be pregnant.
Sit tight, and grab some cookies, because we?re about to go deep into lactation.
First up: how do hunks of tissue make milk?
The anatomy of a breast:
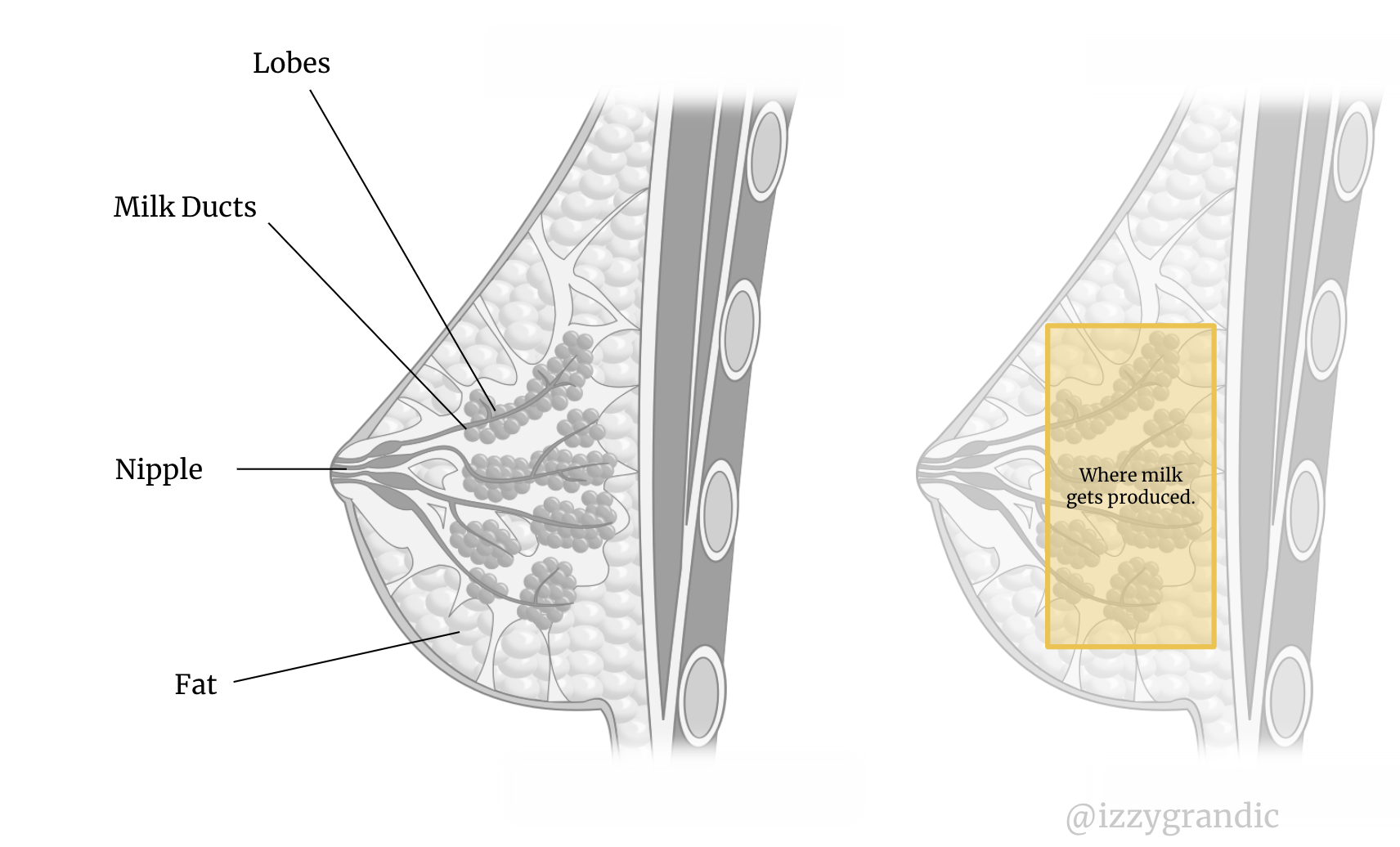
While you?re pregnant, the surge of estrogen and progesterone get your fatty tissue and milk ducts excited. The milk ducts grow in quantity and size. (Each breast may get 1.5 pounds heavier, but it varies).
Estrogen and progesterone trigger the breast-enlargement process. Yet, prolactin is the real MVP for breast milk production. (Its name means ?pro? ?milk production (lactation)? ).
(There are other hormones that might play a role in this process, but we don?t understand them. Scientists think insulin, thyroxine and cortisol may play a role).
When a newborn suckles their mother?s breast, they trigger prolactin to make more milk.
What do women make all this milk from? Their diets?
Actually, no. Breast milk isn?t a complete reflection of mom?s dietary choices because it?s made from blood.
What are the steps to make milk from blood?
Step 1: suck.
When the infant sucks the nipples, the brain releases milk-making hormones.
Fun fact: the breasts have glands, called Montgomery glands, which produce a protective oil. This oil keeps the breasts sanitary & clean for the baby. Don?t put any fancy creams on there; it?ll ruin the protective oil!
Step 2: Make milk
These hormones trigger the alveoli cells to make milk.
Prolactin ? triggers the alveoli to take nutrients from your blood. Other hormones help transport other ingredients, but we don?t fully understand their function. It takes 400L-800L of blood to make 1L of milk.
Step 3: send it!
We?re still using hormones?
Oxytocin ? causes alveoli to send milk down the breast?s milk ducts.
And, then the infant gets its milk. Woo!
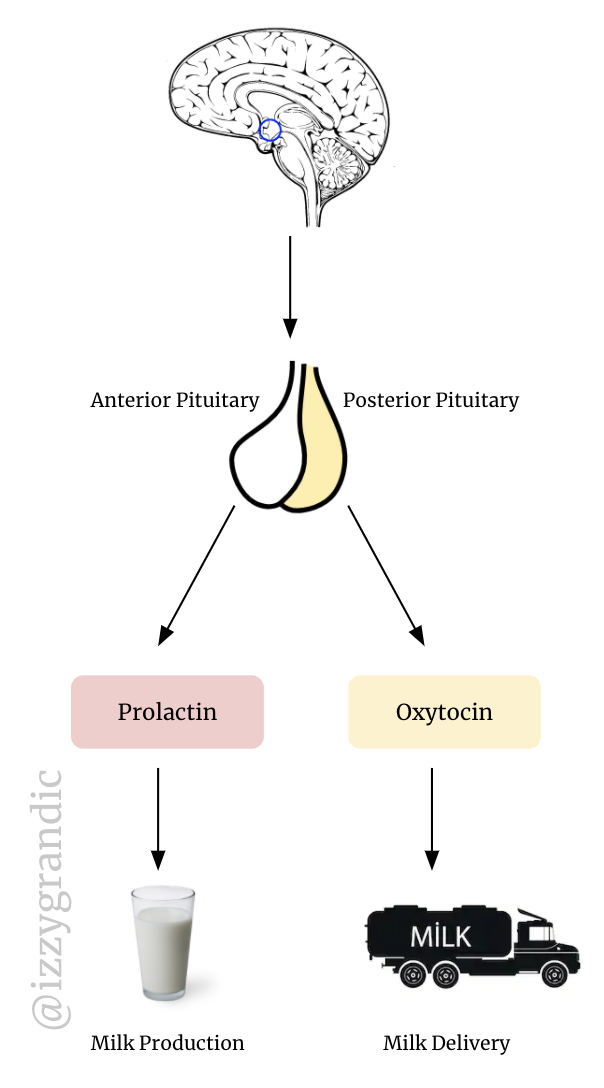
Milk production changes over time. There are 3 types of breast milk:
- Colostrum: milk produced in the first 2?3 days. The mother produces very small amounts of milk, but it is thick and nutrient-packed. This is the ?starting trial? of the milk.
- Transition: day 7?14 the mother starts producing thinner milk in larger quantities.
- Mature: after 2 weeks milk is ?mature,? which means it?s even thinner than transitional milk. It also contains more antibodies and immune system protection.
Breast milk is the best natural formula for a baby for its first 6 months of life. It contains:
- Immune boosting cells
- 1000+ proteins and 20 amino acids
- 200+ complex sugars (oligosaccharides) ? no wonder they call them complex.
- 40+ enzymes
- Growth factors, hormones, vitamins and minerals.
- Antibodies and immune protection. Note: this is something that baby formula does not provide.
- 1 400 microRNAs which help regulate and protect the baby?s gene expression.
It?s like a magic potion for a baby?s development.
Breast milk changes over time, and it can actually change daily. It?s adaptable. For example, when a mom gets sick, she passes her antibodies from that sickness to the baby.
Some women choose to feed their baby formulas instead of milk, which has its own set of risks. It might be more convenient, but formula milk isn?t as adaptable and immune-protective as breast milk.
Nipples will get injured.
For the first few months, mothers are a full-time milk machines; breastfeeding 7?9 times per day.
Having an infant nag at one?s breasts several times a day becomes sore, very quickly.
Especially if they?re doing it wrong. The way an infant latches onto the nipples matters. If it does so in the ?wrong? way, it will cause avoidable nipple pain.
Having the wrong nipple latch is like wearing your shoes on the wrong foot. Painful and avoidable.
Let?s talk about nipple pain. How do we solve it?
- Changing how the baby grips the nipple.
- Changing positions. In sports, people have their go-to ?position;? whether it?s a soccer striker or a basketball shooting guard. Before you find your favourite position, you need to try many out.
- Replenish nipples after feeding. Between feeding, there are different techniques that help reduce pain later.
- Use protective equipment like breast shells.
- Last resort: patience. The body will *hopefully* get used to the pain soon.
C?o?w? human breast pumps
Remember the male inventors that thought women were cows? And they decided to model human breast pumps after cow breast pumps?
Well, the good news is, they?re somewhat more user friendly!!
Breast pumps let women store their breast milk. They work by stimulating the nipples the same way infants do.

Now, let me be clear. Breast pumps traditionally have not been elegant, fun nor comfortable. They?ve allowed working women to provide their children with milk more conveniently. But, there?s tons of room to grow.
As a first-time mom (or even a repeat mom!), you might not be an expert in breastfeeding latches or air-drying your nipples. There are so many new changes happening in your world; it?s hard to keep up.
One of the largest things I?ve noticed in the pregnancy/nursing realm is its overload of information.
THERE IS SO MUCH GOING ON AND SO MUCH INFO TO FILTER THROUGH. +100 bonus points to every mom out there for going through childbirth and nursing. I?ve only watched a few graphic youtube videos, and I still felt some pain.
There are definitely people more versed than I am in boob-pain help; this article is a good starting point to learn more.
Menopause.
Menopause is a permanent breakup with fertility.
Women stop ovulating (releasing an egg), which means there?s nothing for sperm to fertilize.
If there?s no fertilization, there?s no zygote, blastocyst, embryo, fetus or newborn.
And, bonus points, a woman?s period stops.
But, it?s not as bonus-full as it seems. Menopause is difficult, painful and hormonal (notice this theme in women?s health yet?).
I wrote a more in-depth article about menopause here.
A woman?s fertility doesn?t disappear overnight. It can slowly decline over several years to a decade.
Women go through Pre-menopause, or ?perimenopause.?
Perimenopause is like touching a chilli pepper then touching your nose and eyes.
 Or someone else?s face. Either way, it sucks for the ?touched? person.
Or someone else?s face. Either way, it sucks for the ?touched? person.
At first, it tingles.
You think: ?It?s not too bad.?
Then, it gets a little more irritating. The burning sensation increases.
And it gets worse.
And worse.
So, you splash some water.
No.
That.
Wasn?t.
A.
Good.
Move.
At.
ALL.
Your face is a chilly pepper.
You feel like your face peeling away.
You start to write your will.
You think it?s over. It feels over. The sensations are overwhelming. You are the Australian Forrest fires.
Then, you read enough Reddit threads to know to splash milk in your face to relieve the sensation. Now you?re bathing your face in cow breast liquid.
The tingling remains, but it is more manageable. It takes the burning 30 minutes to settle. They?re the longest 30 minutes of your life.
*end scene*
So, that?s a graphic metaphor for perimenopause.
If perimenopause is getting a chilly pepper in your nose, menopause is like suffering a fourth-degree burn.
(I?ll let you google what a fourth-degree burn looks like)
Before getting into the ?hot? stuff, let?s set the scene. Women can experience menopause in 2 ways:
- Naturally: women will stop ovulating as they get older. This can happen between the age of 40?62. The one year anniversary of her last period is the official start of menopause.
- Artificially: some dramatic [usually medical] event prevents the reproductive system from ovulating. For example, if we remove a woman?s ovaries, she is physically unable to release her eggs. Or, if we cause damage through chemotherapy, we can induce menopause.
This metaphor isn?t only figurative ? it?s literal. Menopause is hot.
75% of women experience periods of uncontrollable burning sensations. If they happen during the day, we call them hot flashes, if they happen during the night, they?re night sweats.
For minutes at a time, women will feel as though their entire internal body is on FIRE.
The vagina loses its edge, and sex drive goes down.
When women have their menstrual cycles, they have hormones monitoring their reproductive region all the time. Hormones do this because they want to promote ?sexual activity? while the woman is still fertile.
To do so, sex has to feel good. To feel good, the vagina has to be in solid shape.
But when you?re no longer fertile, reproduction (and sex) aren?t a priority for your body. Your biological energy should be used elsewhere to keep you alive.
TLDR: the vagina declines in function, and sex hurts (which can lower your drive).
It hurts to do things that were normal before, like peeing.
The pelvic floor muscles become weaker.
You pee your pants a little more often.
Insomnia
As your body starts to malfunction, you?ll have more trouble going to sleep.
The heat flashes don?t help. Neither does constant need to go to the bathroom. Nor any type of pain down-there.
61% of women report sleep problems.
Say goodbye to bone density.
Women lose 30% of their bone mass within 5 years after menopause.
Walking will hurt. Doing anything with movement will hurt more.
Brain fog & mood changes.
Two significant things will happen: your memory becomes worse, and you become extremely emotional.
Now?s a good time to transition to why this all happens.
321? hormones.
For a woman?s adult life, she lives in a hormonal rhythm. She does this for decades. Then one day, all those hormones (basically) stop. That?s a drastic change.
In particular, post-menopausal women lack estrogen and progesterone.
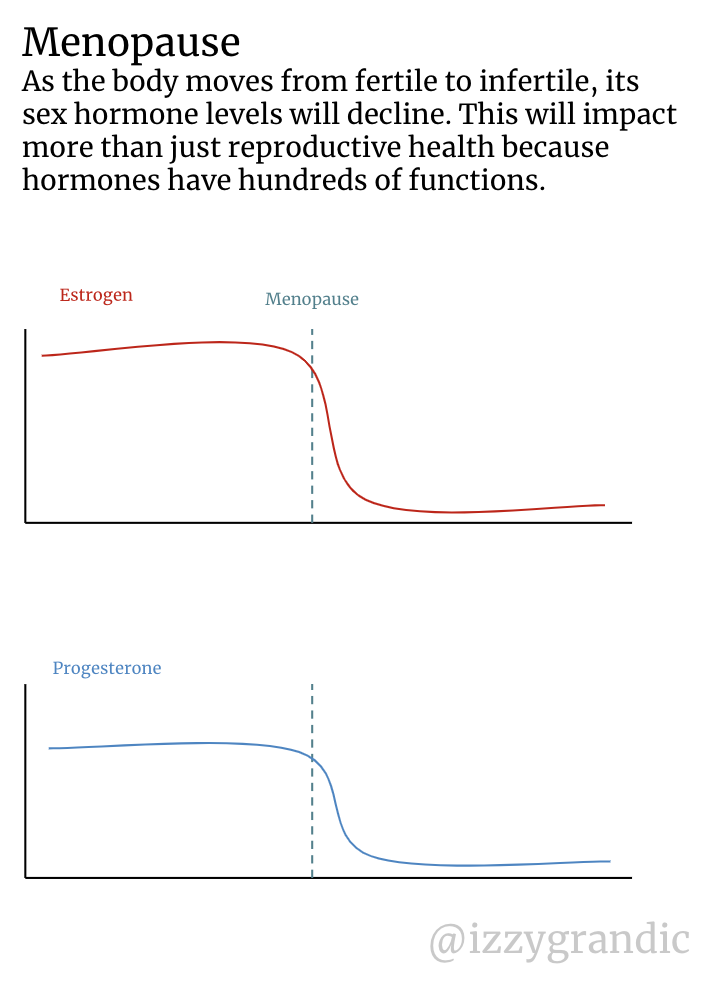 These hormone levels drop dramatically
These hormone levels drop dramatically
Imagine you?re a math professor, and one day you?re never able to use a calculator again. It will be difficult to do things you?ve been doing for years or decades. You?ll never be the same math professor again.
Now, I want to be careful and clear about linking a lot of women?s health ?issues? to hormones. Hormones, inherently, are not a problem. They are the only reason anyone gets to be alive in the first place. Most importantly, they don?t make women inferior.
But, they can be intense, especially if we can?t control them. It?s hard to control something we can?t understand.
Women are hormonal; and it?s a beautiful thing. But holy heck would it be nice to have a sliver of hormonal support sometimes.
I cannot count on one hand the number of times I?ve bought a pet fish during my PMS out of a weird impulse. Only to find out it was the pesky estrogen impulsing me all along when my period started a few days later.
Female Only Diseases
As long as I can remember, school taught me that boys and girls are equal, and should be treated equally. We deserve equal pay, equal opportunities and equal chances.
I started to think that boys and girls were different sides of the same coin.
Here?s the thing: boys and girls aren?t created equal, they?re created differently.
Biologically, we are not the same. Neither of us is ?inferior? or ?superior.?
Good and bad don?t exist, humans made it up; it?s a story. Human rights are a story. Politics are a story. Equality is a story. Fundamentally, none of these things exist anywhere in the order of the world.
But, humans are bad at separating stories from reality, so we believe them anyway. Sometimes stories change ? like the story of equality over time ? but we almost always are telling some sort of story.
The story of equality has killed women.
For the hundreds of thousands of years, humans have viewed men as superior to women. We?ve spent most of our culture and history idolizing men, and building things suited for men.
This still holds true today. Females with their seatbelt on are 73% more likely to get injured in a frontal car accident than males with their seatbelt on.
In the last hundred or so years, we?ve (mostly) stopped considering women as property. Which means, they desire rights. The rights and service women got were equal to the rights/service of men. Because they wanted equality, so they got it.
This included having good healthcare. The same healthcare as men.
Yet, women and men are fundamentally different, why should they receive the same care? Women are not men with boobs. But, our textbooks still use white, heterosexual men as the ?universal body? to study in medicine.
Repairing a bike is different than repairing a tow-truck. Why bring them to the same mechanic?
There are problems beyond reproduction for women. Let?s talk about them. Now.
Diseases are sex-specific.
We know that men and women are somewhat different. Almost every biological function I?ve written about here is exclusive to women. Men can?t get pregnant, have periods or go through menopause. The fact that women can do these things influences their health in other ways.
Certain diseases occur more often in women than in men. Let?s look at some examples.
Women get MS (multiple sclerosis) 4X more often than men.
2/3 of Alzheimer?s patients are women.
Women are 1.38X more likely to report neck pain.
If a disease is more prevalent in one gender, we need sex-specific treatments.
To solve something, you need to target its root cause. If you don?t attack the root, then the problem will reappear. Like, if you cut the top of a plant, it?ll regrow, but if you root it, it won?t.
We need to root health problems to solve them.
But, if a disease is, say, 4X more common in women than men, the root cause can?t be the same. Something different is going on in women that quadruples their chance of suffering from that disease.
If the root cause was the same, the disease would be 50/50 experienced. We rarely see this in practice.
Men and women are like different types of ?cakes.? For the sake of example, men are red velvet cake, women are strawberry cheesecake.
Both are cake. Both have a large audience of people who enjoy them. But, their recipes are different.

If both cakes were too sweet, we wouldn?t (necessarily) use the same ?treatment? to unsweeten them. They?re made of different ingredients, at different ratios.
We should study each cake, and determine its unique root causes of the sweet taste. The solutions would very likely be different.
The healthcare system today is solving strawberry cheesecake?s problems with red velvet?s solutions. Gordon Ramsay would slap our healthcare system.
There are two problems holding our cake-perfecting system behind:
- We don?t test women as often, and we don?t know their symptoms as well, or what makes them different. Historically women were in <20% of clinical trials. In some areas of medicine it?s getting better, in others, it?s not.
- We diagnose them later. For a database of 770 diseases, women get diagnosed ~4 years later. For cancer it?s 2.5, for metabolic diseases it?s 4.5. One of the only exceptions is osteoporosis.
We?re getting a bit better at #1. We?ve started to tell the difference between men’s and women?s symptoms.
Half of women with heart failure get the wrong treatment
- Women?s blood vessels age faster than men?s. Their circulatory system is different.
- Women experience less ?heart attacks? than men. Their heart failure is caused by slow malfunction and stiffening of the heart. Often, this happens after menopause when estrogen levels drop.
- Symptoms appear differently in women, some doctors can?t even recognize it. The wait time to diagnose & receive treatment is longer, and, there are fewer treatments recommended to them. They?re less-frequently prescribed treatments like statins.
Female athletes 1.5?2X more likely to injure their ACL (knees) ? which can be a lifelong and career-ending injury.
- Estrogen makes the ACL ligaments weaker, and more prone to injury. More ACL injuries happen during a girl?s period (when her estrogen levels are highest).
- Studies found that birth control pills reduced the risk of injuring ACL. Why? The pill ?levels out? estrogen. This means there?s less ?intense? periods of high estrogen, which make the ACL vulnerable.
Adrenal Cancer is 3x more prevalent in women than men.
- The adrenal gland is a hormone-producing gland right above the kidneys
- Female adrenal cells turnover 3x faster than males. Different things are going on.
- Scientists think the nature of the adrenal cells in women vs men account for the key differences.
Women are 2X as likely to have asthma (after puberty)
- Men have 10X the amount of testosterone, which decreases inflammation in lung cells.
- When there?s less testosterone more lung cells release cytokines. They are signalling proteins that can cause inflammation. Inflammation of the lungs makes breathing more difficult.
Autoimmune diseases are more common among women because they have less testosterone
- Testosterone is ?protection? for autoimmunity. Autoimmunity is when your body attacks your healthy cells as if they?re foreign invaders.
- B cells can release harmful antibodies that attack cells. Testosterone suppresses a protein called BAFF. BAFF helps B-cells survive.
- So: less testosterone = less BAFF = less B cells.
Scientists are starting to discover the key differences between men and women. Here are some recent examples:
- Men and women respond to stress differently.
- Women are more likely than men to get UTIs.
- Women are more susceptible to concussions because their brain nerve fibres are thinner.
- Men and women have different navigational systems.
We?re also learning about the role of important female sex hormones, like estrogen beyond reproduction.
- After menopause, the drop in estrogen causes teeth loss and other dental problems. We?re starting to correlate menopausal symptoms to potential other problems. A study found that periodontal diseases (tooth loss) are correlated with hypertension.
- Hormone exposure is important for mental health. The longer women are exposed to estrogen in their lifetime, the more they?re protected from depressive or mood disorders.
- & for other diseases, like type 2 diabetes. The longer the exposure to sex hormones, but later in life, reduces the risk of type 2 diabetes.
What?s the implication for all this?
I see 2 main implications:
- We shouldn?t look for universal disease treatments. Doctors, researchers and innovators need to consider sex differences.
- The hormonal and reproductive lifestyle of a girl is an important deciding factor for future diseases. And, we barely know anything about the long-term impacts of hormones. It?s a high potential research area.
Everything has to start somewhere.
8,000 (ish) years ago, curious humans tried squeezing cow boobs, and now we have a $673.8B dairy market.
I think we?re starting to ?squeeze the boobs? of the women?s health sector. There are already some exciting players/ideas in the space, but I know we can go further and do more with femtech.
Femtech Companies
Before we wrap off, I wanted to share some companies in each of the topics I mentioned. This is definitely not a comprehensive list, just a starting point for the very curious 🙂
Hopefully someday soon I?ll have a strong database with more women?s health-centric companies? it?s coming !!
Menstruation
Freda, Rael, Lola, Ohne, Easy, Cora: Organic Period-product Market Places
Honey Pot Company: herbal + bacteria-killing products like tampons and menstrual cups.
Daye: CBD infused tampons for pain relief
Aurat Raaj: chatbot for girls age 10?16 in Pakistan
Oky: UNICEF funded app for girls in Mongolia, and less-targeted period product markets.
Clue, Flo, Glow: general period trackers
Next Gen Jane: smart tampons to predict endometriosis and cervical tampons
Contraception
Natural Cycles: digital birth control
Evofem: Innovative contraception, such as maintaining pH in the vagina at levels that inhibit sperm mobility. In phase 3 clinical trials.
Inne: Hormone mini lab which can be used to understand when it is safe/unsafe to have sex if you don?t want to become pregnant.
Pill Club: a platform to prescribe and fill birth control.
Pexxi: AI for finding the right contraceptive
Conception
Ava: fertility bracelet
Bonzun: AI and Software for IVF
Carrot: fertility benefits
Extend Fertility: several fertility services like IVF, embryo freezing and egg freezing
Ovusense: a medical device for body temperature monitoring to track fertility
Modern Fertility: test to understand personal fertility, and make decisions based on hormones
Pregnancy
Bloomlife: remote, prenatal care
HeraMed: Digital Pregnancy Monitoring
Mahmee: tracking health records between a mother and physicians.
Ninepluslife: on-demand doula support during pregnancy
Nursing
LactApp: breastfeeding support app
Elvie: silent breast pump
Coroflo: monitoring breastfeeding volumes and ensuring babies are eating enough
Menopause
KaNDy Therapeutics: non-hormonal menopause symptoms
Gennev: telemedicine and support for post-menopausal women
Damiva: vaginal moisturizer to get over the vaginal deterioration
Female diseases
Kheiron: transforming breast cancer diagnostics with AI
?Still searching for more examples of companies in this category. If anyone has any examples, please let me know!!v
Investing in women?s health isn?t only about improving healthcare and decreasing illness. It?s also about economic empowerment and building confidence/independence in women.
Let?s Recap ? What are the key things you should take away?
- Women work on cycles. We?re really predictable ? or at least we should be. Cycles are good indicators of health, beyond just fertility. We should be actively monitoring women?s cycles.
- Hormones control everything! The good, the bad, and the ugly. But, there are still so many mysteries in how they work.
- At any given stage of an adult woman?s life, she?ll experience some level of pain. There is always some way to make female life better.
- Giving women power over their fertility is an economic investment. It?s not only giving them control over their bodies, but it gives them control over their careers.
- Women?s health and men?s health are different, with overlap. They?re not created equally. We should invest in both.
- We can daydream about 100% effective contraception, and pain-free labour, but most of the world doesn?t have access to the female health luxuries that exist today. We should still focus on advancing research and understanding, but there?s a huge untapped market for affordable women?s health problems.
There are 3.87B women in the world. 600M girls are going through puberty and starting their periods. 2B menstruate. 100M women are pregnant right now. There will be 56M abortions this year. 25M will go through menopause this year. 1.2B will be post-menopausal by 2030.
Let?s milk this opportunity ?.
Hi, I?m Izzy! I?m a 16-year-old science & tech nerd. Feel free to connect or ask questions!
- [email protected]
- Twitter | Linkedin | Website
PS. You might be interested in some of these articles I?ve written.
? A guide to Menopause
? The Foundation of Femtech
? Reproducing Reproduction
? Female-Centric Reproductive Diseases
? Why Pregnant Women are Moody
? 11% of Women are Internally Bleeding
? Why we age and why we might now have to anymore

