And what it teaches us about addiction and compulsion
 Photo by Get Budding on Unsplash
Photo by Get Budding on Unsplash
Our attitude towards marijuana has shifted drastically in the past century. An era of fear-mongering and government intervention has long passed, giving way to a predominantly liberal culture which embraces the drug for both medicinal and recreational use. This increasingly tolerant stance is largely responsible for an unprecedented rise in marijuana use, especially among adolescents and young adults.
Medical literature is still catching up with the widespread consumption of marijuana. THC and CBD, the two major components of the drug, act on a wide range of organs including the brain, GI tract, and immune system: a series of targets known collectively as the endocannabinoid system. Although medical science has known about this system since the late 1980s, there is still much left to understand about how chronic marijuana use affects the body.
One emerging complication that has just recently been documented is cannabis hyperemesis syndrome. This fascinating disorder suggests that for some users, marijuana is not the benign drug it is often portrayed to be. But it also gives us an important case study to examine topics pertaining to addiction, substance abuse, and compulsive behavior.
Mystery diagnosis
Cannabis hyperemesis was first described in a 2004 case study involving 9 patients who presented to the emergency room with symptoms of cyclical vomiting: recurring attacks of profuse vomiting, nausea, and abdominal pain. Upon further investigation it was revealed that each patient had been using marijuana multiple times a day for at least a year prior to the onset of symptoms. They were not diagnosed with any psychiatric disorders.
Fluid replacement therapy and anti-emetic drugs (emesis refers to vomiting in Latin) were prescribed to the patients as per the standard treatment regimen. But curiously, a hot shower or bath was consistently found to be the most effective treatment, alleviating their symptoms within minutes. This activity quickly became something of a compulsive symptom for the patients:
A novel finding was a ?compulsive bathing? or washing behaviour noted in nine of 10 patients (X, Y, A, Q, R, J, K, E, and G). These patients would have multiple hot showers or baths on the ward. This ritual became the patients primary preoccupation, with them often waking at night to perform it.
Given the patients? extensive use of marijuana and strange bathing habits, the authors of this 2004 study concluded that their symptoms were not confined to cyclical vomiting. They coined the name cannabis hyperemesis syndrome to describe the condition, which exhibits the following 3 essential features: symptoms of cyclical vomiting, compulsive bathing, and symptom resolution on cannabis cessation. Since this original report, many other studies have been published which document this bizarre disorder.
The hypothalamic dysregulation hypothesis
There are two intriguing questions we can ask in light of cannabis hyperemesis. The first is how marijuana, a drug that is frequently prescribed to treat nausea, can have the paradoxical effect of inducing vomiting in high doses. The second is why bathing with hot water should help to alleviate symptoms, an observation which is unique to cannabis hyperemesis and is not found in any other disorders involving vomiting and nausea.
The consensus among researchers is that marijuana induces a dysregulation of the hypothalamus, a part of the brain responsible for a variety of autonomic functions including thermoregulation, feeding, and satiety. Like many other parts of the brain, the hypothalamus contains neurons which express CB1 and CB2, the two main receptors of the endocannabinoid system.
 The hypothalamus is responsible for many autonomic functions
The hypothalamus is responsible for many autonomic functions
Why should taking a hot shower alleviate the symptoms of the disorder? One theory involves TRPV1 neurons in the skin, which are responsible for sending information about heat and acute pain to the brain and have been shown to project to the hypothalamus. Stimulating these nerves may somehow be correcting the dysregulation caused by the metabolites of marijuana. Alternatively, washing oneself with hot water may divert blood from the gut and into the skin, causing alterations in the digestive system that ease symptoms of nausea and abdominal pain.
As for the paradoxical finding that marijuana induces vomiting, it is suspected that the drug actually has two effects: one on the central nervous system (the brain and spinal cord) and another on the peripheral nervous system (all other nerves in the body). The antiemetic effects of marijuana are caused by its action on the brain, whereas its action on the gut seems to delay gastric emptying, inducing nausea and vomiting. Cannabis hyperemesis may occur under high concentrations of marijuana when the peripheral effects override its more well-known central ones.
A vicious cycle
Two kinds of patients are apparent from the literature on cannabis hyperemesis. The first are ?responsive? patients, who understand that marijuana is the cause of their symptoms and promptly abstain from the drug. Due to their cessation of marijuana, symptoms do not return and they are no longer readmitted to the hospital.
The second type, however, is more interesting. These patients react poorly to the idea that marijuana is causing their symptoms, sometimes insisting that doctors are simply obligated to advise against the drug. As a result, they are frequently discharged from the hospital only to return weeks or months later for renewed symptoms of debilitating vomiting and abdominal pain.
For these patients, the decision to continue using marijuana results in a cyclical pattern of symptoms which researchers have divided into three distinct phases: the prodromal phase, the hyperemetic phase, and the recovery phase.
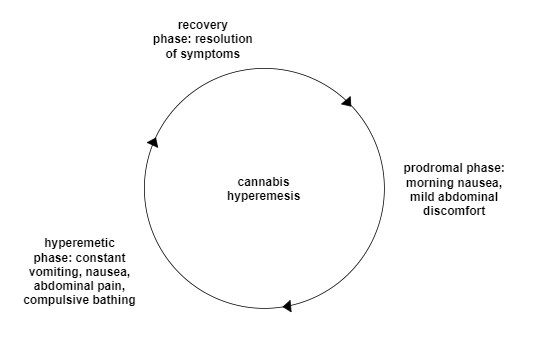
The prodromal phase refers to the onset of symptoms, which usually manifest as nausea especially during the morning and a ?fear of vomiting?. In addition, patients may suffer from mild abdominal discomfort.
Symptoms become acute during the hyperemetic phase: this is the period when patients usually admit to the hospital, as their vomiting becomes so debilitating that it interferes with their daily lives. Many patients also suffer from nausea and abdominal pain. Patients are known to begin compulsively showering during this phase. In addition, patients typically lose anywhere from 5?10 pounds due to dehydration and loss of appetite.
Finally, all symptoms are resolved during the recovery phase, whereupon patients are discharged from the hospital. As symptoms subside, the patient will often regain the weight that was lost during the symptomatic phase. As is standard, doctors inform their patients that abstaining from marijuana is the only way to ensure that their symptoms do not reappear.
This cycle of ER visits, debilitating vomiting, and compulsive bathing is repeated over the course of several weeks or months. It can be made even more pronounced when patients continue to smoke during the prodromal phase, believing that marijuana will help their symptoms of nausea. Additionally, THC is highly lipid-soluble and can remain in fat cells for long periods of time. This may produce a so-called ?reintoxication effect? whereby blood levels of THC rise when the patient loses weight during the recovery phase.
Patients who are caught in this cycle drain an enormous amount of resources from the emergency departments that they choose to visit. One study estimated that the average patient?s overall cost incurred is upwards of $75,000, between fluid replacement therapies, imaging, and boarding. Continued use of marijuana is a lose-lose for both the patients and the hospitals treating them.
An epidemic?
No doubt, conservative voices will be quick to emphasize the rise of cannabis hyperemesis, a disorder which opposes the popular conception of marijuana as a benign drug. Researchers believe that this diagnosis is being severely underreported due to lack of education. One study showed that the incidence of cannabis hyperemesis has doubled since Colorado legalized the drug in 2015.
Moreover, cannabis hyperemesis does suggest that ?cannabis toxicity? is a real medical condition. High levels of THC or its secondary products seem to be interfering with with hypothalamus? ability to regulate temperature and gut activity. As the consumption of marijuana increases globally, it will be important to investigate the long-term impacts of chronic marijuana use, and cannabis hyperemesis is one example of this.
 Photo by Alex Person on Unsplash. Dispensaries like this one are becoming more common in the US
Photo by Alex Person on Unsplash. Dispensaries like this one are becoming more common in the US
However, it?s important for us to take a step back and understand this condition in its context, lest we fall into the all too pervasive tendency to sensationalize. Cannabis hyperemesis only effects those who use marijuana multiple times a day over the course of many years. This represents a very small proportion of overall marijuana consumption.
In addition, cannabis hyperemesis seems to have a genetic component. Not every habitual smoker of marijuana develops symptoms, even when use is heavy and sustained. Specifically, researchers have pointed to variations in the P-450 enzyme as a potential factor in one?s likelihood for developing the syndrome.
In other words, as a medical phenomenon, cannabis hyperemesis is hardly an epidemic. However, I believe that the disorder can teach us interesting things about how we view addiction and compulsion.
Addiction and the limits of behavior-based diagnostics
Sports gambling is a growing industry with many enthusiastic participants. It can be an exciting hobby for those with a predilection for math and statistics, in addition to those who want to earn some money from their sports expertise.
But as we all know, a small proportion of people suffer from a pathological relationship with gambling. Rather than being a positive activity, sports gambling can be a source of significant pain for this group, interfering significantly with their daily life and well-being. At a certain point, we?re willing to venture that their relationship with gambling is indicative of a mental disorder.
How can we distinguish between the gambling enthusiast and the gambling addict? The DSM-5, the standard for psychiatric diagnoses in the United States, defines a gambling disorder under the following diagnostic criteria:
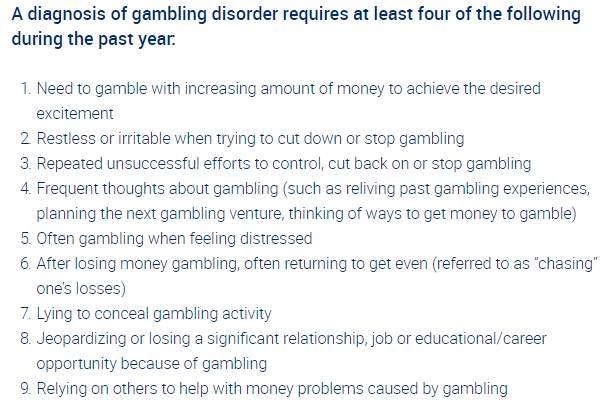
Descriptive passages like these are common in the DSM-5. An aggregate of a patient?s thoughts and behaviors are catalogued precisely and the diagnosis is given on the basis of these activities ? in this case, 4/9 being present. The difference between pathological and non-pathological gambling, then, is whether a person?s engagement with it results in those behaviors or not.
But we should be suspicious of this behavior-based approach to mental health. One popular example should suffice here: if a patient comes into a clinic wanting to be cured of his neurotic symptom of counting windows, he shouldn?t be happy if the treatment simply displaces the illness and has him counting cars instead.
In other words, there is a dimension of addiction that stands beyond simply the level of activity. When it comes to consuming marijuana, this can be understood as the opportunity cost: what the patient is not doing by choosing to use the drug at any particular time
 Photo by Thought Catalog on Unsplash
Photo by Thought Catalog on Unsplash
In the case of cannabis hyperemesis, I think we can identify the opportunity cost in the act of compulsively bathing. In other words, the decision to keep using marijuana should be understood as an unwillingness to part with this symptom. What this leaves us with is an inverted conception of cannabis hyperemesis, where the bathing is what drives the smoking, and not the other way around.
What is so precious about the act of compulsively bathing? It may be that it gives the patients an illusory notion of control: that their health is in their hands, and thus no critical examination of their marijuana use is necessary. Consequently, their decision to consume marijuana is sustained by the eventuality of this false solution: the anticipation of its arrival is what drives the addict to continue using.
The relationship between extreme nausea, compulsive bathing, and symptom resolution in cannabis hyperemesis is a complicated one. I?ve tried to describe the disorder in a way that goes beyond the simple behavior-based standard of the DSM. Cannabis hyperemesis is a fascinating case study on substance abuse and addiction for which further research is necessary. And in the meantime, if you know anyone presenting with symptoms of the disorder, tell them to kindly put the joint down.
Subscribe to my newsletter for updates on future articles: https://pages.convertkit.com/e8233d5800/cb92edd54d