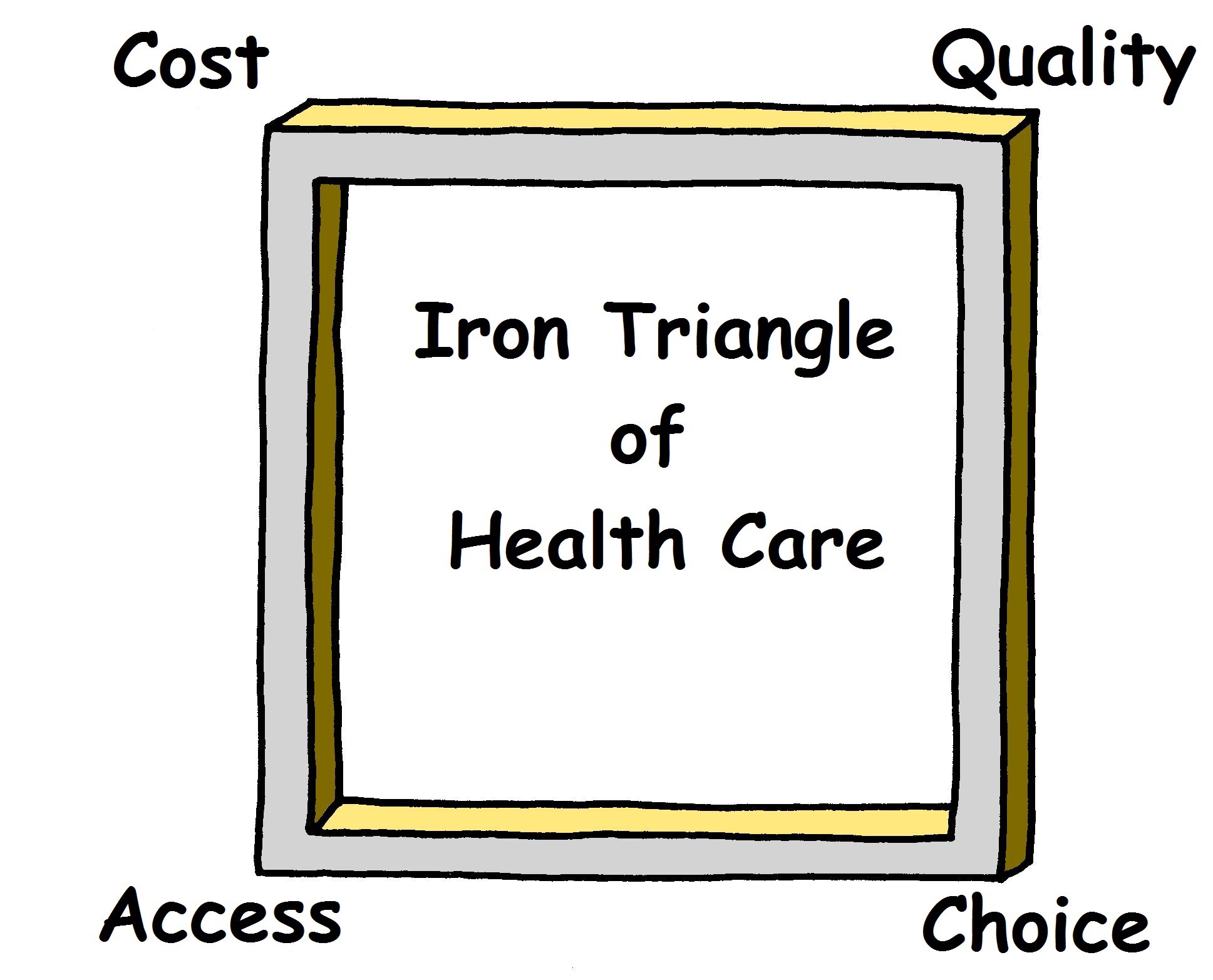
The Iron Triangle of Health Care is a concept developed by William Kissick, the father of Medicare, in his 1994 book, Medicine?s Dilemmas: Infinite Needs Versus Finite Resources. He describes three health care issues which are the primary concerns of all health care systems and that operate in a dynamic and complex relationship: Cost, Quality, and Access. The Triangle is Iron because it is generally difficult to have a low-cost, high quality, wide access health care system. It is generally assumed that if quality increases, then costs must increase as well. And, as you can see below, some commentators argue that Choice is the fourth corner of the Triangle, which, I suppose, would make it an Iron Square.
 source cc
source cc
Below we will briefly explore each of the corners of the Iron Polygon of Health Care. In a future post, we will examine how different countries around the world have designed their health care systems and made compromises within the Iron Polygon.
Cost
The most simple of the corners to understand. This is merely a question of how much does health care cost. The goal is always to reduce cost as much as possible because that allows more people to afford health care which leads to a more healthy and productive population.
But the ways in which costs are contained is where it gets interesting. In the US, many of us are familiar with private insurance as a way to lower costs by spreading risk and cost around the population. But insurance has been around for a long time; the Chinese invented it 5,000 years ago.
 Warmonger, Peacenik, Social Engineer
Warmonger, Peacenik, Social Engineer
A more recent innovation comes from the 19th century Prussian, Otto von Bismarck. Yes, the same Bismarck for whom the short-lived German battleship was named. In a Bismarckian health care system, health care prices are set by the national or state authorities. This manages costs through price controls.
An even more recent innovation has occurred in the US under Medicare and EPO plans. Despite the wide, and growing, prevalence of this innovation, many Americans are not aware of what it is or what it is called. This cost control mechanism is capitation. Under capitation, when a patient is assigned to a doctor, that doctor will receive a flat annual or monthly fee for that patient no matter how many times that patient sees the doctor. This creates a predictable price for health care services and incentivizes doctors to figure out how to deliver higher quality health care (so they don?t have to see their patient as often) at a flat price.
Cost is the corner which demands compromise on all of the other corners of the Iron Polygon. Cost considerations drive down potential quality, and limit access and choice. Innovations in managing cost are important, but these innovations are driven by how they interact with one or more of the other corners.
Quality
Quality is also one of the seemingly more simple corners. This is a measure of how good of health care is being delivered to patients. But health care is a broad thing, and many different aspects of it are subject to quality measures.
For example, we could ask how good are the inputs. As in, how good are the surgeons, how good are the primary care docs, how good of drugs can you buy, do you have the latest surgical robots, how sensitive are your MRI machines, how meticulous are your pathologists, etc.
But how good of drugs you can buy might not always be the most relevant question for measuring quality. For a long time, the main quality measure in, for example, cancer care has been, what is the 5-year survival rate. In other words, what percentage of patients who are diagnosed with a specific type of cancer at a specific stage of that cancer will still be alive in 5 years. This has the benefit of being relatively easy to measure. But the physical and mental toll of cancer treatment can be excruciating. To provide a more balanced measure of health care quality, various groups have been developing health-related quality of life (HRQoL) assessments with the goal of measuring how different treatments affect patients? quality of life (e.g., Health-related quality of life and cancer clinical trials).
Quality can be difficult to measure, but you generally get what you pay for and high quality is generally expensive (yes, there are exceptions, particularly by brilliant physicians at foreign AMCs).
Choice
Choice was not one of the corners of Kissick?s Triangle. But the trend in health care over the past 20+ years has been towards patient-centered care. The goal of patient-centered care is to care for patients in the context of their own social worlds, and make them feel listened to, informed, respected, and involved in their care.
The theory, and the research that backs up the theory, shows that if patients are empowered with knowledge of their condition and are allowed to meaningfully participate in their health care decisions, then there is greater buy-in by the patient. This buy-in results in patients who are engaged and who manage their health and medical conditions more responsibly.
For example, if a patient is informed about the amount of and type of rehab they must perform before and after knee surgery, and if the patient understands why they have to perform so much rehab, then the patient is more likely to do their rehab, which means that the patient will have a more successful knee surgery.
In patient-centered care, the personal and professional relationship between the patient and their physician is very important because a patient and a physician with a good relationship are more likely to make good mutual decisions than patients and physicians with a bad relationship. Thus, a patient?s ability to choose their health care provider becomes an important part of a health care system.
In countries with single-payer health care systems, such as England, or for people in the US with EPOs or HMOs, patients do not have much choice of health care provider. In the US, that has long been the benefit of having a PPO insurance plan: you have the choice of physician. But choice comes with costs, and single-payer systems sacrifice that choice for broad access.
Access
Access is the most nebulous of the corners because access means a lot of things. At its most simple, access asks whether you can access the type of health care that you need. In the US, we generally see this framed as an urban/rural divide. There a lot of doctors in urban areas, but patients in rural areas often need to travel a long distance to see specialists. Patients in rural areas then don?t have reasonable access to specialty care.
In developing countries, by comparison, one of the questions that is asked is what percentage of the population can access a surgical center within 2 hours.
But access is not just the single question of do you have a doctor nearby. Cost plays a major role in access. If health care is too expensive to afford, then people lack access due to affordability. If health care is so low quality as to be ineffective, then people lack access to effective health care (in the ancient world people generally got better health outcomes by praying to Zeus and drinking amethyst dust to cure a migraine than paying a quack doctor to drill a hole in their head). And if the only doctor you can see with reasonable travel is one that you do not like, then you are unlikely to access that doctor.
Every developed country in the world, except the United States, has designed their health care systems around maximizing access to health care. Compromises are made on choice and quality to minimize cost in order to allow as many people as possible to access care at a price that is affordable to the government, employers, and citizens.
In the United States, health care has been heavily regulated, but we have never tried to implement a general health care system until the Patient Protection and Affordable Care Act (ACA). The main goal of the ACA has been to broaden access through the individual mandate to be covered by insurance, while managing costs through mandated private insurance and some limits on choice, while maintaining the high quality health care that America is renowned for.
But maintaining high quality health care at a reasonable cost is a difficult task. That is why the core driver of health care innovation in the US, and around the world, is to develop new tools to improve quality, access and choice at minimal additional cost.
William Lewis is General Counsel at MORE Health where he manages the company?s legal risks in global health law, corporate governance, and cybersecurity. MORE Health delivers patients access to the best physicians in the world when they need it the most.
![[123MoviE] Watch Pet Sematary ONLINE 2.0.1.9 (HD-1080p) Full and FrEe 4K](https://911weknow.com/wp-content/themes/mts_myblog/images/nothumb-myblog-related.png)